Understanding Secondary Traumatic Stress & Vicarious Trauma
What are secondary traumatic stress and vicarious trauma differences risk factors and management? It’s a question many helping professionals grapple with. We’re all familiar with the impact of trauma on those directly experiencing it, but what about the ripple effect? This post dives into the often-overlooked realities of secondary traumatic stress (STS) and vicarious trauma (VT), exploring their distinct characteristics, the factors that increase vulnerability, and crucially, how to manage and prevent them.
Let’s unpack this complex yet vital topic together.
We’ll be looking at the core differences between STS and VT, examining their symptoms, and exploring how various risk factors, both personal and environmental, contribute to their development. We’ll also delve into effective management strategies, including evidence-based interventions and preventative measures for individuals and organizations. The goal? To equip you with a deeper understanding of these issues and the tools to navigate them.
Defining Secondary Traumatic Stress (STS) and Vicarious Trauma (VT)
Understanding the differences between secondary traumatic stress (STS) and vicarious trauma (VT) is crucial for professionals and individuals who work with those experiencing trauma. While both involve experiencing the emotional consequences of another’s trauma, they manifest differently and require distinct approaches to management.
Core Characteristics of Secondary Traumatic Stress
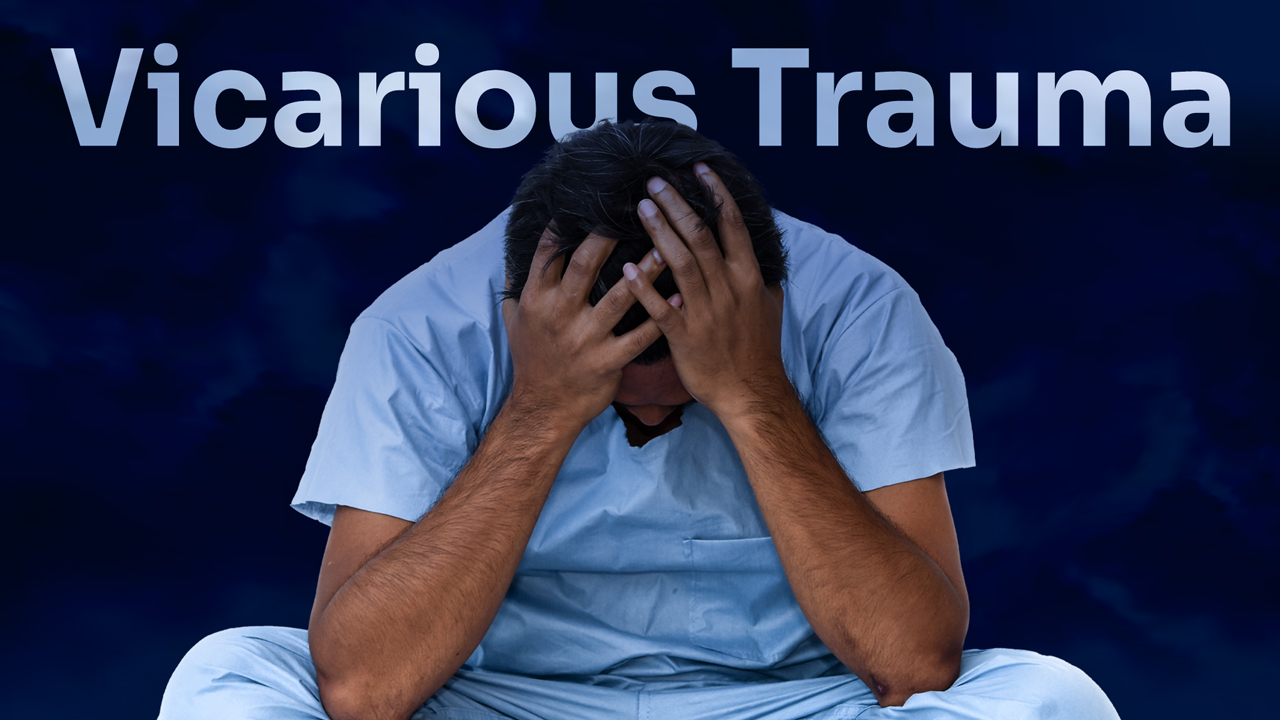
Secondary traumatic stress (STS) refers to the emotional duress caused by exposure to the traumatic experiences of others. It’s a natural consequence of bearing witness to or learning about the suffering of another person. The core characteristic of STS is the development of symptoms similar to those experienced by individuals who have directly experienced trauma, but without the direct exposure to the traumatic event itself.
The intensity of STS symptoms often correlates with the intensity and duration of exposure to the traumatic material. It’s important to note that STS is not a sign of weakness; it’s a predictable response to significant emotional burden.
Key Differences Between STS and Vicarious Trauma
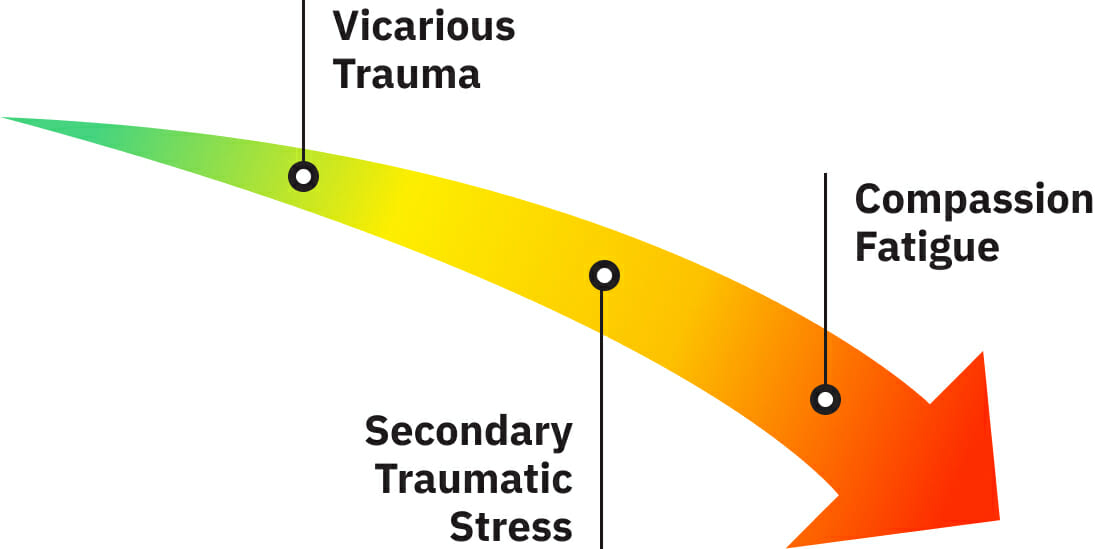
While both STS and VT stem from exposure to trauma, they differ in their core mechanisms. STS primarily involves experiencing stress symptoms as a result of exposure to another’s trauma. The focus remains on the
- impact* of the trauma on the individual experiencing STS. In contrast, vicarious trauma (VT) is a more profound and lasting change in one’s worldview and beliefs, a fundamental shift in how one perceives the world and one’s place in it. VT is less about experiencing the
- symptoms* of trauma and more about experiencing a
- transformation* of one’s fundamental beliefs and values. This transformation often involves a loss of hope, cynicism, and a diminished sense of safety and security.
Symptom Comparison of STS and VT
The following table compares and contrasts the symptoms of STS and VT. The severity columns represent a general trend and can vary significantly based on individual factors and the nature of the exposure.
| Symptom | STS Severity | VT Severity | Distinguishing Features |
|---|---|---|---|
| Intrusive thoughts/images | Mild to moderate; fleeting | Severe; persistent and pervasive | STS intrusive thoughts relate directly to the client’s trauma; VT intrusive thoughts may be more generalized and relate to a sense of disillusionment. |
| Anxiety/Irritability | Moderate; episodic | Severe; chronic | STS anxiety is often situationally triggered; VT anxiety is more pervasive and can be a constant state. |
| Sleep disturbances | Mild to moderate; temporary | Severe; persistent insomnia or nightmares | STS sleep issues are often directly related to exposure; VT sleep disturbances may be related to a pervasive sense of unease. |
| Emotional numbing | Mild; situational | Severe; pervasive and persistent | STS numbing is often a coping mechanism; VT numbing reflects a fundamental shift in emotional capacity. |
| Feelings of helplessness/hopelessness | Mild to moderate; episodic | Severe; chronic and pervasive | STS feelings of helplessness relate to the client’s situation; VT feelings of helplessness are often generalized and reflect a loss of faith in the world’s capacity for good. |
Situations Leading to STS and VT
Several situations can lead to the development of STS and VT. For example, a therapist working with clients who have experienced severe trauma, such as sexual assault or war, is at a high risk of developing STS. The constant exposure to graphic details and emotional distress can lead to the development of symptoms. Similarly, emergency responders, social workers, and healthcare professionals who regularly encounter traumatic events are also at risk.
VT, on the other hand, may develop over a longer period of time through repeated exposure to traumatic stories or situations. It’s often associated with a profound sense of disillusionment, a loss of hope, and a feeling of being overwhelmed by the suffering of others. For instance, a human rights lawyer working with victims of genocide for many years may experience VT due to the constant exposure to immense suffering and the feeling of powerlessness to alleviate it.
Risk Factors for STS and VT
Source: amazonaws.com
Understanding the factors that contribute to the development of secondary traumatic stress (STS) and vicarious trauma (VT) is crucial for effective prevention and intervention. These factors are complex and often interact, creating a heightened vulnerability in some individuals and professions. While not everyone exposed to trauma will develop STS or VT, recognizing these risk factors allows for proactive strategies to support those at greater risk.
Individual Risk Factors for STS and VT
Pre-existing mental health conditions significantly increase the likelihood of developing STS and VT. Individuals with a history of anxiety, depression, or PTSD are more susceptible to the emotional impact of exposure to others’ trauma. Similarly, certain personality traits can play a role. For instance, individuals with high levels of empathy and a strong sense of responsibility may be more prone to absorbing the emotional distress of others.
These individuals might find it difficult to establish healthy boundaries, leading to increased risk. A predisposition towards emotional reactivity or difficulty regulating emotions can also amplify the impact of exposure to trauma narratives.
Understanding the differences between secondary traumatic stress and vicarious trauma, including their risk factors and management strategies, is crucial for those working with trauma survivors. The emotional toll can be significant, and sometimes it feels like we’re facing our own insurmountable challenges, much like the incredible hurdles overcome in developing organ transplantation, such as the recent news that the fda approves clinical trials for pig kidney transplants in humans.
This highlights the importance of self-care and seeking support to mitigate the potential impact of vicarious trauma on mental health. Proper management is key to preventing burnout and maintaining well-being.
Social and Environmental Risk Factors for STS and VT, What are secondary traumatic stress and vicarious trauma differences risk factors and management
The workplace environment plays a crucial role in shaping vulnerability to STS and VT. A culture of high stress, inadequate supervision, limited resources, or a lack of support systems can exacerbate the impact of exposure to traumatic material. For example, healthcare professionals working in high-pressure environments with limited access to peer support or debriefing may be at increased risk.
Similarly, social isolation, lack of a strong support network, and limited access to mental health services can increase the likelihood of developing STS or VT. The absence of a supportive community that validates the emotional toll of the work can significantly impact an individual’s ability to cope.
Interactions of Risk Factors
The interaction between individual and social risk factors can create a potent combination that increases vulnerability. For example, a healthcare professional with pre-existing anxiety and a history of family trauma working in a high-pressure emergency room with limited support might be at significantly higher risk of developing STS or VT than someone without these factors. The cumulative effect of these stressors can overwhelm coping mechanisms, leading to the development of these conditions.
Consider a social worker dealing with child abuse cases; if they possess high empathy but lack adequate supervision and debriefing opportunities within a demanding workload, the likelihood of developing STS or VT increases substantially.
Understanding the differences between secondary traumatic stress and vicarious trauma, including their risk factors and management, is crucial for caregivers. The emotional toll can be significant, and sometimes, managing the stress of a child’s condition like Tourette Syndrome adds another layer of complexity. For helpful strategies in managing Tourette’s in children, check out this great resource: strategies to manage tourette syndrome in children.
Returning to the initial topic, effective self-care is key to mitigating the impact of secondary trauma and vicarious trauma on caregivers.
Protective Factors for STS and VT
Understanding protective factors is just as important as identifying risk factors. These factors can mitigate the impact of exposure to trauma and reduce the risk of developing STS or VT.
- Strong social support network: Having supportive colleagues, friends, and family members who provide emotional validation and practical assistance is crucial.
- Effective coping mechanisms: Developing healthy coping strategies such as mindfulness, exercise, and engaging in enjoyable activities can help manage stress and prevent emotional overwhelm.
- Access to professional support: Regular access to mental health professionals who provide specialized training in trauma-informed care can offer crucial support and guidance.
Manifestations of STS and VT
Understanding the ways secondary traumatic stress (STS) and vicarious trauma (VT) manifest is crucial for effective prevention and intervention. While there’s significant overlap, subtle differences exist in their presentation, influenced by individual factors and the specific nature of exposure to trauma. Recognizing these manifestations allows for targeted support and promotes the well-being of those at risk.
Emotional Manifestations of STS and VT
Both STS and VT frequently involve a range of emotional disturbances. Individuals might experience persistent sadness, anxiety, irritability, and difficulty concentrating. Feelings of helplessness, hopelessness, and emotional numbness are also common. However, a key difference lies in the focus of the emotional distress. STS often centers on the client’s trauma and the worker’s concern for their well-being, while VT involves a more profound shift in the individual’s worldview, leading to feelings of disillusionment and a sense of personal vulnerability.
For example, a social worker experiencing STS might feel overwhelmed by the sheer number of cases involving child abuse, while experiencing VT might question their own capacity for empathy and compassion after prolonged exposure.
Psychological Manifestations of STS and VT
The psychological impact of STS and VT can be profound. Intrusive thoughts, nightmares, and flashbacks related to the clients’ trauma are possible in STS. In VT, the psychological impact often manifests as a pervasive sense of cynicism, distrust, and a decreased capacity for joy. Individuals may experience difficulty forming healthy attachments or struggle with feelings of guilt and shame, even when not directly responsible for the client’s trauma.
For instance, a healthcare worker experiencing STS might have nightmares about a particularly difficult patient’s injuries, whereas someone experiencing VT might withdraw from social interactions and develop a negative outlook on humanity.
Physical Manifestations of STS and VT
The physical toll of STS and VT is often significant and shouldn’t be overlooked. Common symptoms include fatigue, insomnia, headaches, gastrointestinal problems, and a weakened immune system. These physical manifestations often reflect the underlying emotional and psychological distress. While both STS and VT can present with these symptoms, the intensity and persistence might differ. A social worker with STS might experience temporary fatigue after a particularly demanding caseload, whereas someone with VT might experience chronic fatigue and sleep disturbances.
Presentation of STS and VT in Different Professional Groups
The presentation of STS and VT can vary across professional groups depending on the nature of their work and the types of trauma they are exposed to. Healthcare workers, for example, might experience STS and VT related to witnessing patient suffering, death, and injury. Their symptoms might include heightened anxiety about patient well-being and a sense of emotional exhaustion.
Social workers, on the other hand, might experience STS and VT related to exposure to clients’ stories of abuse, neglect, and violence. Their symptoms might include feelings of powerlessness, disillusionment, and a sense of moral injury. The intensity and type of symptoms will vary depending on individual resilience, coping mechanisms, and the level of support available.
Visual Representation of STS and VT Symptoms
Imagine a Venn diagram. The two overlapping circles represent STS and VT. The overlapping area contains symptoms common to both, such as anxiety, fatigue, insomnia, and difficulty concentrating. The area unique to the STS circle could include symptoms directly related to clients’ trauma, such as intrusive thoughts or nightmares about specific cases. The area unique to the VT circle could contain symptoms reflecting a change in worldview, such as cynicism, detachment, and a decreased sense of hope.
The diagram illustrates the shared and distinct manifestations of STS and VT, highlighting the complexity of these conditions.
Management and Treatment Strategies for STS and VT
Source: vetintegrations.com
Secondary Traumatic Stress (STS) and Vicarious Trauma (VT) can significantly impact mental health and well-being. Fortunately, various evidence-based interventions are available to help individuals manage and mitigate these conditions. Effective treatment often involves a combination of therapeutic approaches and self-care strategies tailored to individual needs and preferences.
Evidence-Based Interventions for Managing STS
Managing STS effectively requires a multifaceted approach. Therapy, particularly those focusing on trauma-informed care, plays a crucial role. Cognitive Behavioral Therapy (CBT) helps individuals identify and challenge negative thought patterns and develop coping mechanisms for stress. Eye Movement Desensitization and Reprocessing (EMDR) can be particularly effective in processing traumatic memories experienced indirectly through exposure to others’ trauma narratives.
Mindfulness-based interventions, such as meditation and yoga, promote self-awareness and emotional regulation, crucial skills in managing the overwhelming emotions associated with STS. Self-care strategies, such as regular exercise, healthy eating, sufficient sleep, and engaging in enjoyable activities, are also essential components of a comprehensive STS management plan. These practices help build resilience and prevent burnout.
Evidence-Based Interventions for Managing VT
Vicarious trauma, unlike STS, often involves a deeper, more pervasive impact on the individual’s sense of self and world view. Peer support groups provide a safe and validating space for individuals to share experiences, normalize their feelings, and learn coping strategies from others who understand. Trauma-informed supervision is critical for professionals regularly exposed to traumatic material, providing a supportive environment to process vicarious trauma and maintain professional well-being.
Self-compassion practices, focusing on self-kindness and acceptance, are vital in counteracting the self-criticism and feelings of inadequacy that can accompany VT. Furthermore, engaging in activities that foster a sense of meaning and purpose can help individuals rebuild a positive sense of self and reconnect with their values.
Comparing and Contrasting Treatment Approaches for STS and VT
While both STS and VT benefit from therapeutic interventions like CBT and EMDR, the focus and emphasis differ. For STS, the treatment often concentrates on managing symptoms like anxiety, stress, and sleep disturbances. In contrast, VT treatment frequently addresses the more profound impact on the individual’s worldview and sense of self, requiring a more intensive exploration of personal values and beliefs.
Peer support and trauma-informed supervision are particularly valuable in addressing the relational and existential aspects of VT. Both conditions benefit from self-care strategies, but the intensity and type of self-care may need tailoring to the specific challenges posed by each condition. For example, someone experiencing VT might benefit from more profound self-reflection and activities that reconnect them with their sense of purpose.
Understanding the differences between secondary traumatic stress and vicarious trauma, including their risk factors and management strategies, is crucial for mental health. It’s fascinating to consider how seemingly unrelated areas connect; for instance, research suggests that early detection of dementia, as explored in this article about whether an eye test can detect dementia risk in older adults, can eye test detect dementia risk in older adults , might indirectly impact the stress levels of caregivers who may be at increased risk of these conditions.
Returning to the initial topic, effective management involves self-care and professional support.
Resources and Support Systems for Individuals Experiencing STS and VT
Accessing appropriate support is crucial for managing STS and VT. A list of resources includes professional help from therapists specializing in trauma and vicarious trauma, peer support groups, and online resources offering information and support.
- The National Child Traumatic Stress Network (NCTSN): Offers resources and training on trauma-informed care and support for professionals and families.
- The Substance Abuse and Mental Health Services Administration (SAMHSA): Provides a national helpline and a wealth of information on mental health services and support.
Prevention Strategies for STS and VT: What Are Secondary Traumatic Stress And Vicarious Trauma Differences Risk Factors And Management
Preventing Secondary Traumatic Stress (STS) and Vicarious Trauma (VT) is crucial for maintaining the well-being of professionals who work with trauma survivors. A proactive approach, encompassing organizational policies, individual self-care, and comprehensive training, significantly reduces the risk of these debilitating conditions. This involves a multi-faceted strategy targeting both the work environment and the individual’s coping mechanisms.
Organizational Preventative Measures
Organizations play a vital role in mitigating the risk of STS and VT. Implementing robust preventative measures demonstrates a commitment to employee well-being and fosters a healthier, more productive work environment. These measures should be integrated into the overall organizational culture and not viewed as an add-on.
- Regular Debriefing Sessions: Structured debriefing sessions, facilitated by trained professionals, provide a safe space for employees to process their experiences and emotions after exposure to traumatic material. These sessions should focus on emotional regulation, normalization of reactions, and identifying potential warning signs of STS or VT.
- Access to Mental Health Resources: Providing readily available and confidential access to mental health services, including counseling and Employee Assistance Programs (EAPs), is essential. Employees should feel comfortable seeking help without fear of stigma or reprisal.
- Workload Management and Caseload Limits: Implementing strategies to manage workloads and prevent burnout is crucial. Setting realistic caseload limits and providing adequate administrative support can significantly reduce stress levels.
- Supervisory Support and Training: Supervisors should receive training on recognizing the signs of STS and VT in their team members and on providing appropriate support and guidance. This includes creating a culture of open communication and encouraging employees to seek help when needed.
Self-Care Practices in Preventing STS and VT
Self-care is not a luxury; it’s a necessity for professionals working in trauma-informed fields. Prioritizing self-care significantly reduces the risk of developing STS and VT by building resilience and promoting emotional well-being.
- Mindfulness and Meditation: Regular practice of mindfulness and meditation techniques can help regulate emotions, reduce stress, and improve overall mental well-being. Even short, daily sessions can make a significant difference.
- Physical Exercise and Healthy Diet: Engaging in regular physical activity and maintaining a balanced diet are fundamental aspects of self-care. These activities contribute to both physical and mental health, improving resilience and reducing stress.
- Social Support and Connection: Maintaining strong social connections and engaging in activities that bring joy and relaxation are crucial for emotional well-being. Connecting with friends, family, or colleagues in a supportive environment can help buffer against the effects of trauma exposure.
- Setting Boundaries and Prioritizing Rest: Learning to set healthy boundaries at work and prioritizing sufficient rest and sleep are vital for preventing burnout and reducing the risk of STS and VT. This includes disconnecting from work after hours and taking regular breaks throughout the day.
Effective Training Programs
Comprehensive training programs are essential for equipping professionals with the knowledge and skills necessary to prevent and manage STS and VT. These programs should go beyond simply informing employees about the conditions; they should equip them with practical strategies for self-care and coping.
- Trauma-Informed Care Training: This training provides a foundational understanding of trauma’s impact and teaches professionals how to provide compassionate and effective care while minimizing their own risk of developing STS or VT.
- Stress Management and Resilience Training: These programs teach practical coping mechanisms, such as stress reduction techniques, mindfulness practices, and self-compassion strategies, to enhance resilience and prevent burnout.
- Vicarious Trauma Awareness Training: This specialized training focuses on educating professionals about the specific nature of vicarious trauma, its signs and symptoms, and strategies for prevention and self-care.
Creating a Supportive Work Environment
A supportive work environment is paramount in preventing STS and VT. This involves fostering a culture of open communication, mutual respect, and a commitment to employee well-being.
- Open Communication and Feedback Mechanisms: Establishing clear channels for communication and feedback allows employees to voice concerns and seek support without fear of judgment or reprisal. Regular team meetings and informal check-ins can help identify potential issues early on.
- Peer Support and Mentorship Programs: Providing opportunities for peer support and mentorship can create a sense of community and shared experience, reducing feelings of isolation and promoting emotional resilience.
- Recognition and Appreciation of Employee Contributions: Acknowledging and appreciating employees’ hard work and dedication fosters a positive and supportive work environment, boosting morale and reducing stress levels.
Final Wrap-Up
Source: ytimg.com
So, understanding the nuances between secondary traumatic stress and vicarious trauma is crucial for anyone working in helping professions or supporting those who are. By recognizing the risk factors, implementing preventative measures, and seeking appropriate support, we can mitigate the impact of these often-invisible burdens. Remember, prioritizing self-care and fostering supportive environments are key to protecting your well-being and maintaining your ability to help others.
Let’s continue the conversation – share your experiences and thoughts in the comments below!
FAQ Explained
What is the difference between compassion fatigue and vicarious trauma?
While both involve emotional exhaustion from exposure to trauma, compassion fatigue is a broader term encompassing burnout and decreased empathy, while vicarious trauma is a more specific type of trauma resulting from exposure to another’s trauma.
Can STS or VT develop gradually over time?
Yes, both STS and VT can develop gradually through prolonged exposure to traumatic material or stressful situations. It’s not always a sudden onset.
Are there specific therapies particularly effective for STS/VT?
Yes, therapies like EMDR, Cognitive Processing Therapy (CPT), and mindfulness-based interventions have shown effectiveness in treating STS and VT. Support groups are also beneficial.
Is it possible to prevent STS and VT entirely?
While complete prevention might be unrealistic, proactive measures like robust self-care practices, organizational support, and regular training can significantly reduce the risk.