What is Histamine Intolerance and How to Manage It
What is histamine intolerance and how to manage it? That’s the burning question for many experiencing unexplained digestive issues, skin problems, or brain fog. Histamine intolerance isn’t a true allergy, but rather a difficulty in properly breaking down histamine, a compound found in many foods and released by the body in response to stress. This can lead to a wide range of symptoms, and understanding the root cause is the first step towards feeling better.
Let’s dive into the world of histamine and discover how to navigate it.
This post will explore what histamine intolerance is, how it differs from a histamine allergy, and the role of enzymes like diamine oxidase (DAO) and histamine methyltransferase (HNMT) in processing histamine. We’ll cover common symptoms, identify high-histamine foods, and delve into effective management strategies, including dietary changes, lifestyle modifications, and when to seek professional help. Get ready to reclaim your health!
What is Histamine Intolerance?

Source: drbeckycampbell.com
Histamine intolerance is a condition where your body struggles to properly break down histamine, a chemical naturally present in your body and many foods. This leads to a buildup of histamine, causing various unpleasant symptoms. It’s important to understand that this is different from a histamine allergy, which involves a more immediate and severe immune system response.
Histamine Intolerance Versus Histamine Allergy
Histamine intolerance is not an allergy. In a histamine allergy, your immune system mistakenly identifies histamine as a threat, triggering an allergic reaction like hives or anaphylaxis. In contrast, histamine intolerance involves a deficiency in the enzymes responsible for breaking down histamine, leading to a slower, less dramatic but often persistent accumulation of histamine in the body. The symptoms are often milder than those of a true allergy, but can still significantly impact daily life.
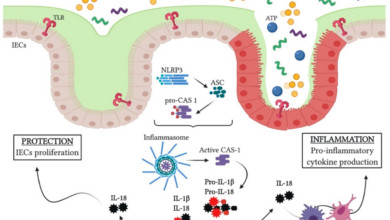
The Role of DAO and HNMT in Histamine Metabolism
Our bodies possess two primary enzymes to manage histamine levels: diamine oxidase (DAO), primarily found in the intestinal lining, and histamine N-methyltransferase (HNMT), found in the liver and other tissues. DAO is responsible for breaking down histamine in the gut, preventing its absorption into the bloodstream. HNMT then further metabolizes the histamine that does enter circulation. A deficiency in either DAO or HNMT, or both, can lead to histamine intolerance, resulting in the accumulation of histamine and subsequent symptoms.
Genetic factors, gut health issues, and certain medications can all influence the activity of these enzymes.
Comparison of Symptoms
The symptoms of histamine intolerance can overlap with other conditions, making diagnosis challenging. The following table helps illustrate some key differences:
| Symptom | Histamine Intolerance | Food Allergy | IBS |
|---|---|---|---|
| Headache | Common | Possible | Possible |
| Skin Rash/Itching | Common | Very Common | Possible |
| Digestive Issues (bloating, diarrhea) | Common | Possible | Very Common |
| Nasal Congestion | Common | Possible | Less Common |
| Low Blood Pressure | Possible | Less Common | Less Common |
| Fatigue | Common | Possible | Common |
| Anxiety/Irregular Heartbeat | Possible | Possible (due to stress) | Possible (due to stress) |
Common Symptoms of Histamine Intolerance
Source: thedempsterclinic.com
Histamine intolerance can manifest in a variety of ways, making diagnosis challenging. Symptoms often overlap with other conditions, leading to delayed or incorrect diagnoses. Recognizing the common symptom clusters can help individuals and healthcare providers better identify potential histamine intolerance. The severity of symptoms can vary greatly depending on individual factors and the amount of histamine consumed or released.
Digestive Symptoms
Digestive issues are frequently reported by individuals with histamine intolerance. These symptoms are often a direct result of the body’s inability to efficiently break down and clear excess histamine from the gut. The resulting inflammation can lead to a range of unpleasant effects.
- Abdominal pain and cramping: This can range from mild discomfort to severe, debilitating pain.
- Bloating and gas: Excess histamine can cause increased gas production and distension of the abdomen.
- Diarrhea: Increased intestinal motility due to inflammation can lead to frequent, loose stools.
- Constipation: Paradoxically, some individuals experience constipation, potentially due to slowed gut motility in response to inflammation.
- Nausea and vomiting: These symptoms are often associated with increased gut inflammation and discomfort.
Skin Symptoms
The skin is another common site for histamine intolerance symptoms to appear. Histamine plays a significant role in inflammatory skin responses, and an excess can trigger various skin reactions.
- Hives (urticaria): These itchy, raised welts are a classic sign of an allergic reaction, often triggered by histamine.
- Eczema: Histamine release can exacerbate existing eczema and trigger flare-ups.
- Itching: Generalized itching or itching in specific areas can be a prominent symptom.
- Flushing: Sudden reddening of the skin, particularly on the face and neck, can occur.
Neurological Symptoms
While less frequently highlighted, neurological symptoms can also be associated with histamine intolerance. The mechanism isn’t fully understood, but the inflammatory effects of histamine can impact the nervous system.
- Headaches and migraines: Histamine is implicated in the pathogenesis of migraines, and excess histamine can trigger or worsen headaches.
- Difficulty concentrating: “Brain fog” and reduced cognitive function are sometimes reported.
- Anxiety and irritability: Histamine’s role in the nervous system can contribute to mood changes.
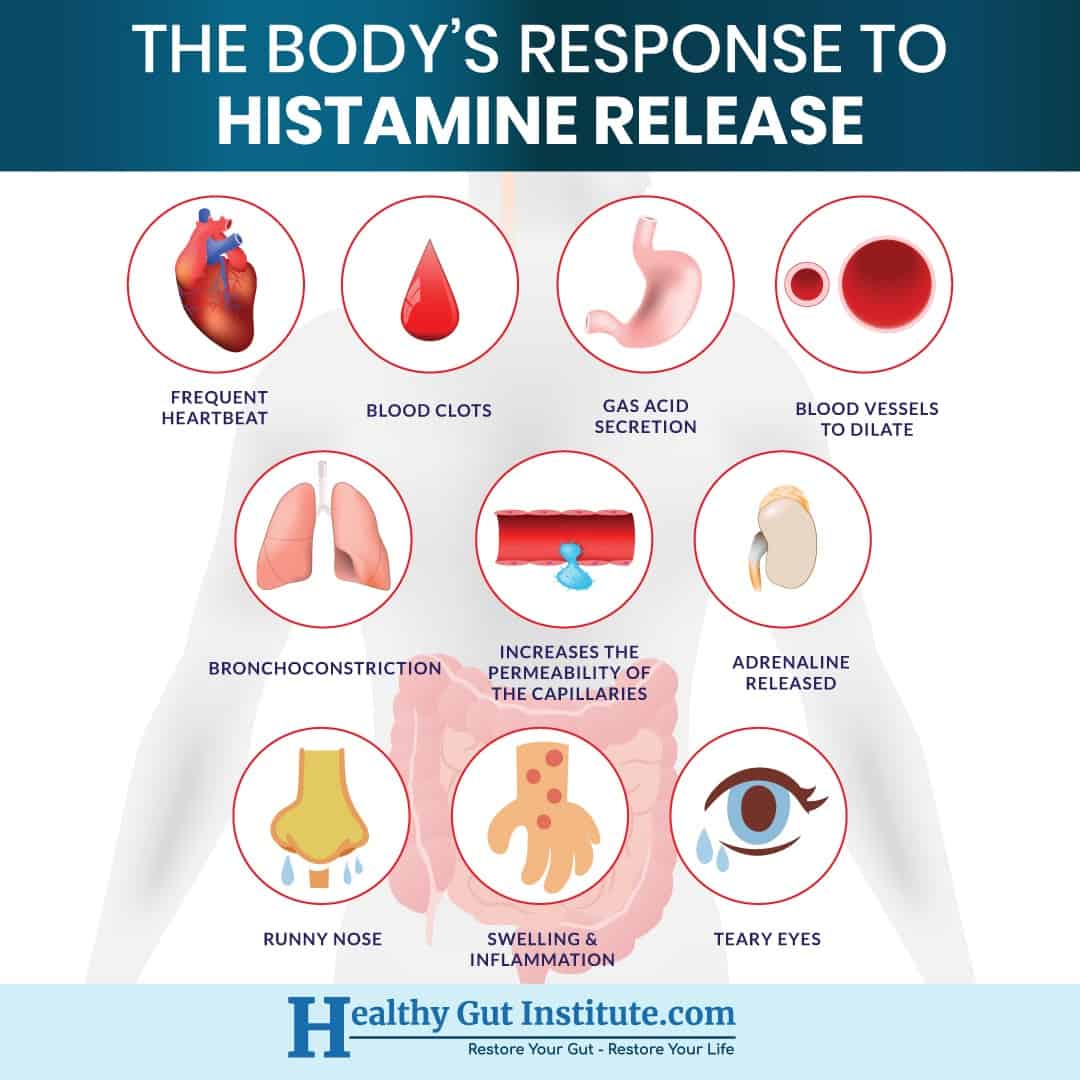
Less Common Symptoms
A range of other, less common symptoms can also be indicative of histamine intolerance. These symptoms often appear in conjunction with the more common digestive, skin, or neurological symptoms.
- Sinus congestion and rhinitis: Histamine release can contribute to inflammation in the nasal passages.
- Watery eyes: Similar to sinus congestion, histamine can affect the eyes.
- Palpitations: In some cases, excess histamine can affect heart rate.
- Low blood pressure: Although less common, histamine can influence blood pressure regulation.
- Muscle aches and pains: Inflammation related to histamine can contribute to muscle discomfort.
Identifying Histamine-Rich Foods
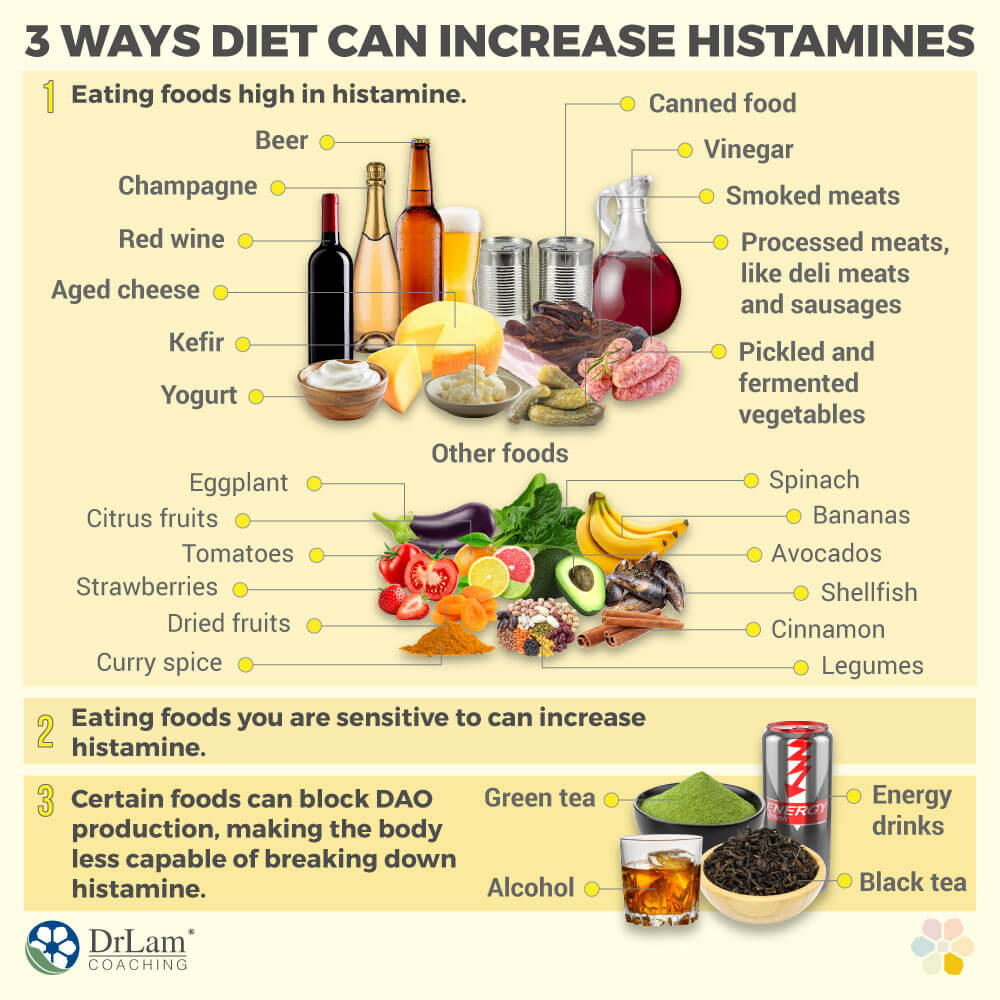
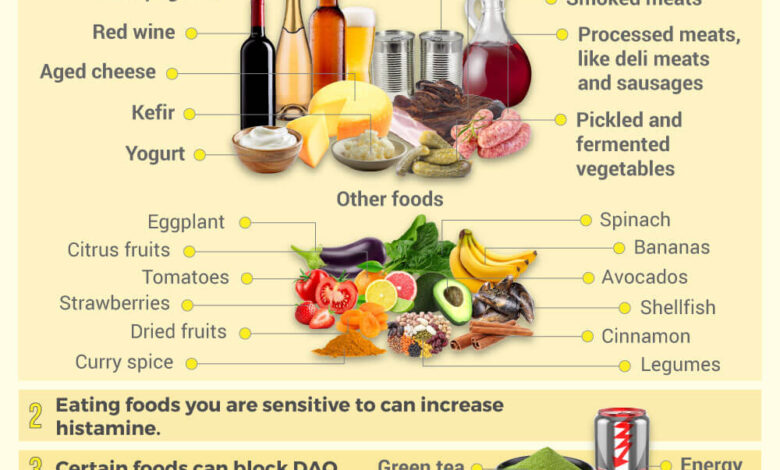
Source: drlamcoaching.com
Knowing which foods are high in histamine is crucial for managing histamine intolerance. This isn’t about completely eliminating all high-histamine foods, but rather about understanding your personal tolerance levels and making informed choices to minimize symptoms. Remember, individual reactions vary greatly.
The amount of histamine in food is influenced by several factors, making it challenging to provide precise numbers. However, a general categorization can be helpful in guiding dietary choices.
High-Histamine Foods Categorized
The following table categorizes common high-histamine foods. It’s important to note that histamine levels can fluctuate based on factors discussed below. This table serves as a general guideline, and individual responses may differ significantly.
| Food Type | Food | Histamine Content Level |
|---|---|---|
| Fermented Foods | Aged cheeses (Cheddar, Swiss, Parmesan), Sauerkraut, Kimchi, Yogurt, Fermented Soy Products (Soy Sauce, Miso) | High |
| Fish & Seafood | Tuna, Mackerel, Sardines, Anchovies, Smoked Fish | High |
| Meat & Poultry | Processed meats (salami, sausage, bacon), leftover meat | Medium to High |
| Fruits | Avocados, Bananas, Spinach, Strawberries, Tomatoes | Medium |
| Vegetables | Eggplant, Mushrooms, Spinach | Medium |
| Dairy | Most aged cheeses, sour cream | High |
| Drinks | Alcohol (especially red wine, beer), Aged vinegar | High |
| Other | Chocolate, nuts (especially peanuts), leftovers | Medium to High |
Factors Increasing Histamine Levels in Foods
Several factors contribute to increased histamine levels in food, making some seemingly low-histamine foods problematic for individuals with histamine intolerance. Understanding these factors is essential for effective management.
Processing: Fermentation, smoking, and pickling processes significantly increase histamine content. For example, fresh tuna has lower histamine than smoked tuna. Similarly, freshly made sauerkraut contains less histamine than commercially produced, aged sauerkraut.
Storage: Improper storage of food allows for bacterial growth, leading to increased histamine production. Leaving food out at room temperature for extended periods increases the risk. This is especially true for perishable items like fish and meat.
Spoilage: Spoiled food contains high levels of histamine. Always check for signs of spoilage, such as unusual odors or discoloration, before consuming food.
Histamine Liberation
Certain foods, even those naturally low in histamine, can trigger the release of histamine in the body. This is known as histamine liberation. This occurs when substances in the food interact with mast cells, causing them to release their stored histamine.
Examples of Histamine Liberators: Many foods containing compounds like tyramine, which is found in aged cheese and fermented products, can trigger histamine release. Other examples include food additives like artificial food coloring and preservatives. Even certain medications can cause histamine liberation.
Histamine intolerance, a common issue, involves managing your diet to avoid high-histamine foods. It’s all about finding that balance, and sometimes, that means researching surprising connections! For instance, the amazing advancements in organ transplantation, like the recent news that the fda approves clinical trials for pig kidney transplants in humans , make me wonder about the impact of such procedures on the body’s overall inflammatory responses, which can certainly be relevant for histamine intolerance sufferers.
Understanding how to manage histamine levels is crucial for overall well-being.
Managing Histamine Intolerance Through Diet
Successfully managing histamine intolerance relies heavily on dietary adjustments. By carefully selecting and preparing your food, you can significantly reduce your histamine intake and alleviate symptoms. This involves understanding which foods are high in histamine, which are low, and how food preparation and storage impact histamine levels.
A Sample Low-Histamine Diet Plan
Following a low-histamine diet requires planning and commitment. This sample plan provides a framework; you may need to adjust it based on your individual needs and tolerances. Remember to always consult with a doctor or registered dietitian before making significant dietary changes.
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Monday | Oatmeal with berries (fresh, not frozen) and a sprinkle of cinnamon | Salad with grilled chicken (ensure it’s fresh and not processed), avocado, and a simple vinaigrette | Baked salmon with roasted asparagus and quinoa |
| Tuesday | Scrambled eggs with spinach | Leftover salmon and quinoa | Chicken stir-fry with low-histamine vegetables (e.g., carrots, zucchini, peppers) and brown rice |
| Wednesday | Yogurt (ensure it’s low-histamine, check the label carefully) with fresh fruit | Lentil soup (homemade, using fresh ingredients) | Turkey meatballs with zucchini noodles |
| Thursday | Smoothie with low-histamine fruits (e.g., bananas, pears) and almond milk | Salad with grilled tofu and a simple vinaigrette | Baked chicken breast with sweet potato and green beans |
| Friday | Whole-wheat toast with avocado | Leftover chicken and sweet potato | Pork tenderloin with roasted Brussels sprouts and mashed potatoes (made from fresh potatoes) |
| Saturday | Breakfast burrito with scrambled eggs and low-histamine vegetables | Chicken salad sandwich on whole-wheat bread (ensure mayonnaise is low-histamine) | Roast lamb with steamed broccoli and carrots |
| Sunday | Pancakes made with low-histamine ingredients (check recipes online) | Leftover roast lamb | Shepherd’s pie with a low-histamine topping (e.g., mashed sweet potato) |
The Importance of Fresh, Properly Stored Food
Histamine levels increase in food over time, especially when exposed to heat, light, and air. Therefore, prioritizing fresh, properly stored food is crucial. Buy fresh produce and consume it as soon as possible. Store food correctly – refrigeration is key for most low-histamine foods. Avoid leaving food at room temperature for extended periods.
Freezing can also help preserve some foods, but always check the effect on histamine content for the specific food. For instance, frozen berries generally contain more histamine than fresh ones.
Fermented Foods and Histamine Intolerance
Fermented foods are a double-edged sword in a low-histamine diet. While some are beneficial for gut health, many contain high levels of histamine. The fermentation process itself produces histamine.Suitable Fermented Foods (Consume in moderation and check for histamine levels): Some traditionally fermented foods, prepared in specific ways, may be tolerated by some individuals. Examples include sauerkraut made from fresh cabbage without added vinegar, and kimchi made with minimal added ingredients and fermented for a shorter period.Unsuitable Fermented Foods: Foods like aged cheeses, most types of cured meats, and many fermented sauces (e.g., soy sauce, fish sauce) are generally high in histamine and should be avoided.
DAO Supplements: Benefits and Drawbacks
Diamine oxidase (DAO) is an enzyme that breaks down histamine in the body. DAO supplements may help some individuals with histamine intolerance by supplementing the body’s natural DAO levels. However, it’s crucial to note that DAO supplements are not a cure for histamine intolerance and should be used under the guidance of a healthcare professional. Potential benefits include reduced symptoms, but potential drawbacks include potential interactions with other medications and individual variations in effectiveness.
Some individuals may experience mild side effects. It is vital to choose high-quality supplements and follow the recommended dosage.
Histamine intolerance can be a real pain, making everyday foods trigger headaches and digestive issues. Managing it involves identifying your triggers and adjusting your diet accordingly, which can be tricky! Interestingly, research is exploring links between physical health and cognitive decline, like this article on whether an eye test can detect dementia risk in older adults: can eye test detect dementia risk in older adults.
Understanding these connections highlights the importance of proactive health management, including careful attention to dietary needs like those with histamine intolerance.
Lifestyle Modifications for Histamine Intolerance Management
Living with histamine intolerance often requires more than just dietary changes. A holistic approach encompassing lifestyle adjustments significantly impacts symptom management and overall well-being. By addressing factors like stress, gut health, exercise, and sleep, you can create a supportive environment for your body to better handle histamine.
Stress Reduction Techniques
Stress significantly elevates histamine levels. When under stress, your body releases cortisol, a hormone that can trigger the release of histamine. This can exacerbate symptoms for those with histamine intolerance. Effective stress management is therefore crucial. Techniques like deep breathing exercises, meditation, yoga, and spending time in nature can help lower cortisol levels and, consequently, reduce histamine release.
Regular practice of mindfulness techniques, even for short periods daily, can significantly improve stress management and overall well-being. For example, a study published in the Journal of Psychosomatic Research showed that mindfulness-based stress reduction significantly reduced cortisol levels in participants. Finding activities you enjoy and incorporating them regularly into your routine is key to long-term stress reduction.
Gut Health and Histamine Intolerance
A healthy gut plays a vital role in histamine metabolism. The gut microbiota, the community of bacteria and other microorganisms residing in your intestines, influences the breakdown and elimination of histamine. An imbalance in gut flora (dysbiosis) can lead to impaired histamine metabolism, increasing symptoms. Strategies to improve gut health include consuming prebiotic foods (like bananas and asparagus) to feed beneficial bacteria, taking probiotic supplements containing strains known to support histamine metabolism, and avoiding unnecessary antibiotic use, which can disrupt the delicate balance of gut bacteria.
Histamine intolerance can be a real challenge, often requiring careful diet management and sometimes medication. Understanding the triggers, like certain foods and environmental factors, is key. Interestingly, managing conditions like this sometimes shares similarities with other neurological challenges; for instance, the approaches to behavioral management in kids with Tourette’s, as detailed in this helpful article on strategies to manage Tourette syndrome in children , highlight the importance of consistent routines and identifying triggers.
Similarly, a consistent approach to diet and lifestyle is vital for managing histamine intolerance.
Increasing fiber intake through fruits, vegetables, and whole grains promotes a healthy gut microbiome, further supporting histamine metabolism. Furthermore, avoiding processed foods and excessive sugar consumption can help maintain a healthy gut environment.
Regular Exercise and Histamine Levels
Regular physical activity, especially moderate-intensity exercise, can positively influence histamine metabolism. Exercise promotes healthy blood flow, which can help in the efficient clearance of histamine from the body. Furthermore, exercise reduces stress levels, indirectly contributing to lower histamine release. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Activities such as brisk walking, swimming, cycling, or even gardening can be beneficial.
Remember to listen to your body and avoid overexertion, as intense physical activity can sometimes trigger a histamine release.
Adequate Sleep and Histamine Regulation, What is histamine intolerance and how to manage it
Sleep deprivation can significantly impact histamine levels. During sleep, your body naturally releases histamine, but inadequate sleep can disrupt this natural cycle and lead to increased histamine levels throughout the day. Aim for 7-9 hours of quality sleep per night. Establish a regular sleep schedule, create a relaxing bedtime routine, and ensure your bedroom is dark, quiet, and cool to optimize sleep quality.
If you struggle with sleep, consider consulting a healthcare professional to rule out any underlying sleep disorders. Prioritizing sleep hygiene is essential for managing histamine intolerance effectively.
When to Seek Professional Medical Advice
Suspecting histamine intolerance can be confusing, as symptoms often overlap with other conditions. Knowing when to seek professional help is crucial for accurate diagnosis and effective management. Delaying medical attention can lead to worsening symptoms and potential complications. This section clarifies when professional guidance is necessary and Artikels the diagnostic process and the roles of healthcare professionals.It’s important to remember that self-diagnosing and treating histamine intolerance can be risky.
While dietary changes can often alleviate symptoms, underlying medical conditions might be contributing to your symptoms, requiring specific treatment.
Diagnostic Tests for Histamine Intolerance
Unfortunately, there isn’t a single definitive test for histamine intolerance. Diagnosis relies heavily on a combination of factors, including a detailed medical history, symptom evaluation, and often, a process of elimination. Your doctor may suggest several approaches to help determine if histamine intolerance is the culprit. These might include:
- Detailed Medical History and Physical Examination: Your doctor will thoroughly review your symptoms, medical history, and lifestyle to identify potential triggers and rule out other conditions.
- Food Diary and Elimination Diet: Keeping a detailed record of your food intake and noting any subsequent symptoms can be incredibly helpful. An elimination diet, where you temporarily remove suspected histamine-rich foods, can reveal if your symptoms improve.
- Blood Tests: While there’s no specific “histamine intolerance” blood test, blood tests can help rule out other conditions with similar symptoms, such as allergies or deficiencies.
- Stool Tests: These tests can assess gut health and identify potential underlying issues that might contribute to histamine intolerance, such as gut dysbiosis (an imbalance of gut bacteria).
- DAO Activity Test: This test measures the activity of diamine oxidase (DAO), an enzyme that breaks down histamine in the gut. Low DAO activity can indicate a potential difficulty in processing histamine.
The Role of Doctors and Dietitians in Managing Histamine Intolerance
A healthcare team approach is often most effective for managing histamine intolerance. Both doctors and registered dietitians play vital roles.
- Doctors: Doctors help rule out other conditions, interpret test results, and provide overall medical guidance. They can also address any co-existing health problems that might worsen histamine intolerance symptoms.
- Registered Dietitians: Registered dietitians are crucial for developing personalized dietary plans to manage histamine intolerance. They can help you identify and avoid histamine-rich foods, create a balanced diet, and ensure you’re meeting your nutritional needs while managing your symptoms.
Potential Complications of Unmanaged Histamine Intolerance
Leaving histamine intolerance unmanaged can lead to several complications. While the severity varies, neglecting the condition can significantly impact your quality of life.
- Persistent and Worsening Symptoms: Untreated histamine intolerance can lead to chronic digestive issues, headaches, skin problems, and respiratory symptoms, significantly impacting daily life.
- Nutrient Deficiencies: Restrictive diets, often necessary to manage histamine intolerance, can lead to nutritional deficiencies if not carefully planned by a registered dietitian.
- Mental Health Impact: The chronic nature of the condition and the limitations it can place on daily life can contribute to anxiety, depression, and frustration.
- Exacerbation of Other Conditions: Histamine intolerance can exacerbate other health conditions, such as migraines, irritable bowel syndrome (IBS), or eczema.
Conclusion
Living with histamine intolerance can feel overwhelming, but armed with knowledge and a proactive approach, you can significantly improve your quality of life. Remember, a low-histamine diet is crucial, but equally important are stress management, gut health optimization, and sufficient sleep. While a tailored approach is best determined with the guidance of a healthcare professional, this guide provides a solid foundation for understanding and managing your symptoms.
Don’t hesitate to reach out for support—you’re not alone on this journey to better health!
FAQ Compilation: What Is Histamine Intolerance And How To Manage It
Can I still enjoy fermented foods with histamine intolerance?
Some fermented foods are lower in histamine than others. Look for those fermented for a shorter time and always opt for fresh, high-quality products. However, it’s best to experiment cautiously and monitor your reactions.
How long does it take to see improvements on a low-histamine diet?
The timeframe varies greatly depending on individual factors and the severity of symptoms. Some people notice improvements within days or weeks, while others may take longer. Patience and consistency are key.
Are there any specific tests to diagnose histamine intolerance?
There isn’t one definitive test. Diagnosis often involves a combination of symptom evaluation, food diaries, and sometimes DAO enzyme testing. A doctor or registered dietitian can guide you through the process.
Is histamine intolerance curable?
There’s no cure, but it’s highly manageable. By following a low-histamine diet and incorporating lifestyle modifications, you can significantly reduce symptoms and improve your overall well-being.