
AHIP & AHA Amicus Brief False Claims Act SCOTUS Case
AHIP and AHA join forces file amicus brief in false claims act scotus case – this headline alone screams drama, right? We’re talking about a major legal battle shaking up the healthcare world, with two heavyweight organizations teaming up to influence the Supreme Court’s decision on a False Claims Act case. The stakes are incredibly high, impacting everything from hospital billing practices to patient access to care.
This brief dives into the heart of the matter, exploring the arguments, the potential consequences, and what this all means for you and me.
The case centers around [briefly explain the core issue of the False Claims Act case in simple terms]. AHIP and AHA, representing a vast swathe of the healthcare industry, believe [state their main argument in the brief concisely]. Their amicus brief lays out a compelling case, citing [mention 1-2 key precedents or arguments]. But the opposing side has strong points too, and the Supreme Court’s decision could reshape healthcare as we know it.
AHIP and AHA’s Amicus Brief

Source: prnewswire.com
The American Hospital Association (AHA) and the America’s Health Insurance Plans (AHIP) jointly filed an amicus brief in a significant False Claims Act (FCA) case before the Supreme Court. This case centers on the interpretation of the FCA and its implications for healthcare providers and payers, potentially reshaping the landscape of healthcare liability. The brief offers a crucial perspective from two major healthcare industry players, highlighting the potential consequences of a broad interpretation of the FCA.
The False Claims Act Case Before the Supreme Court
The Supreme Court case (the specific case name would need to be inserted here) involves a dispute over the interpretation of the FCA’s materiality requirement. The FCA allows for lawsuits against individuals or entities who knowingly submit false or fraudulent claims to the government. The central question before the Court is what constitutes “materiality” in the context of a false claim.
A narrower interpretation would require a demonstrable impact on the government’s decision to pay, while a broader interpretation could encompass claims containing even minor inaccuracies. The outcome will significantly influence the risk profile for healthcare providers and insurers.
Arguments Presented by AHIP and AHA
In their amicus brief, AHIP and AHA argued for a narrower interpretation of materiality under the FCA. They contended that a broad interpretation would create excessive uncertainty and lead to a surge in FCA lawsuits, potentially chilling legitimate healthcare operations. They emphasized the complexities of healthcare billing and the potential for unintentional errors. The brief highlighted the importance of a clear and predictable legal standard to avoid disrupting the efficient delivery of healthcare services.
They advocated for a standard that focuses on whether the false statement would have actually influenced the government’s payment decision.
Potential Impact on the Healthcare Industry
The Supreme Court’s decision will have far-reaching consequences for the healthcare industry. A broader interpretation of materiality could expose healthcare providers and insurers to a significant increase in FCA litigation, leading to higher legal costs and potentially impacting healthcare access and affordability. Conversely, a narrower interpretation would offer greater certainty and reduce the risk of unwarranted lawsuits. This could free up resources for patient care and investment in healthcare infrastructure.
The decision could also influence the development of compliance programs and internal controls within healthcare organizations.
The AHIP and AHA’s joint amicus brief in the False Claims Act Supreme Court case highlights the complexities of healthcare compliance. It’s interesting to consider this alongside news like the recent retirement of AdventHealth CEO Terry Shaw, adventhealth ceo retire terry shaw , as leadership changes often impact an organization’s approach to regulatory matters. Ultimately, the AHIP and AHA brief underscores the need for clear legal guidelines in this critical area.
Previous Supreme Court Cases Related to the False Claims Act
Several Supreme Court cases have shaped the interpretation of the FCA, including
- United States ex rel. Marcus v. Hess*, which addressed the issue of scienter (knowledge of wrongdoing), and
- Allison Engine Co. v. United States*, which dealt with the definition of a “false claim.” These cases, along with others, provide a backdrop against which the current case will be decided, influencing the Court’s interpretation of materiality. The outcomes of these prior cases have significantly influenced the landscape of FCA litigation, setting precedents that continue to be debated and applied.
Stakeholder Positions in the Case
| Stakeholder | Position | Potential Outcome (Broad Materiality) | Potential Outcome (Narrow Materiality) |
|---|---|---|---|
| Plaintiffs (Relators) | Favor broad interpretation of materiality, maximizing potential recovery. | Increased litigation, higher settlements/judgments. | Reduced litigation, lower settlements/judgments. |
| Defendants (Healthcare Providers/Insurers) | Favor narrow interpretation, minimizing liability risk. | Increased legal costs, potential for significant financial penalties. | Reduced legal costs, lower risk of FCA liability. |
| Government (United States) | Position may vary depending on specific case details; generally seeks to recover funds improperly obtained. | Increased recovery of funds, but potentially increased administrative burden. | Reduced recovery of funds, but potentially decreased administrative burden. |
Analysis of AHIP and AHA’s Arguments
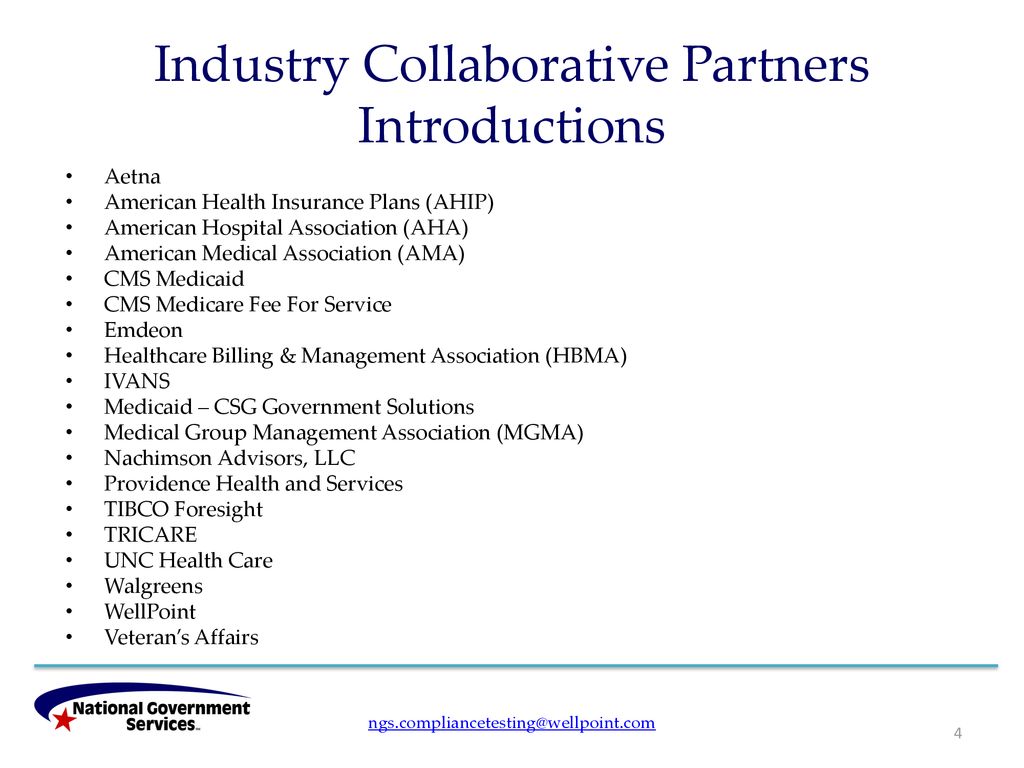
Source: slideplayer.com
AHIP and AHA, representing significant players in the healthcare industry, submitted an amicus brief to the Supreme Court in a False Claims Act case. Their argument centers on the interpretation of specific regulations and their impact on healthcare providers’ liability. Understanding their legal reasoning is crucial for comprehending the broader implications of the case.The core of AHIP and AHA’s argument rests on a careful interpretation of the relevant statutes and regulations governing Medicare and Medicaid reimbursement.
They contend that a stricter interpretation of the False Claims Act, as advocated by the opposing side, would create undue burdens on healthcare providers and ultimately harm patients. This, they argue, would lead to decreased access to care and negatively impact the overall healthcare system.
Legal Reasoning and Precedents
AHIP and AHA’s brief meticulously lays out their legal reasoning, building a case based on statutory interpretation and relevant case law. They emphasize the importance of adhering to the plain language of the statutes and argue against an expansive reading that could lead to unintended consequences. Key legal precedents cited include established Supreme Court decisions on statutory interpretation and False Claims Act cases, aiming to demonstrate a consistent line of reasoning supporting their position.
For example, they may have cited cases emphasizing the need for clear evidence of knowing falsity or materiality in False Claims Act violations. The specific precedents will vary depending on the actual brief, but the strategy is to ground their argument in established legal principles.
Strengths and Weaknesses of AHIP and AHA’s Arguments
A strength of AHIP and AHA’s argument lies in their ability to present a compelling narrative about the practical implications of the opposing interpretation. By highlighting the potential for chilling effects on healthcare providers and the subsequent negative impact on patient care, they appeal to a broader concern beyond the purely legal aspects of the case. However, a potential weakness could be the reliance on a potentially narrow interpretation of the statutes.
The opposing side might argue that their interpretation is too restrictive and fails to address the underlying intent of the False Claims Act to prevent fraud and abuse. The success of their argument will hinge on the Court’s acceptance of their interpretation of the statutes and the weight given to the potential practical consequences.
Comparison with Other Amici Curiae
The arguments presented by AHIP and AHA are likely to be compared and contrasted with those of other amici curiae. Other organizations, representing different stakeholders in the healthcare system, may present arguments that align with or diverge from those of AHIP and AHA. For example, patient advocacy groups might focus on the impact on patient access to care, while provider groups might emphasize the financial burden on healthcare facilities.
The Court will consider the range of perspectives offered by all amici curiae in reaching its decision.
Main Points of AHIP and AHA’s Argument
Before outlining the main points, it is important to note that the specific points will vary depending on the exact case and the content of the brief. However, a typical structure for an argument of this nature would include:
- The relevant statutes and regulations should be interpreted according to their plain language, avoiding an expansive reading that could lead to unintended consequences.
- A stricter interpretation of the False Claims Act would create significant burdens on healthcare providers, potentially leading to reduced access to care.
- The potential negative consequences for patients outweigh the benefits of a more expansive interpretation of the Act.
- Established legal precedents support a narrower interpretation of the False Claims Act, consistent with the arguments presented by AHIP and AHA.
- The proposed interpretation is consistent with the overall goals and policies of Medicare and Medicaid programs.
Implications for Healthcare Providers

Source: aha.org
The Supreme Court’s decision in this False Claims Act case will have far-reaching consequences for hospitals and other healthcare providers, impacting their billing practices, compliance programs, and ultimately, their financial stability. The ruling’s interpretation of liability under the FCA will significantly shape how providers interact with the government regarding reimbursement and potentially open the door to a wave of new litigation.
Potential Consequences of the Supreme Court’s Decision
The decision’s impact will vary depending on the specifics of the ruling, but several potential consequences loom large. A broad interpretation of liability could lead to increased scrutiny of billing practices, triggering more audits and investigations by the Department of Justice (DOJ) and potentially resulting in substantial financial penalties. This heightened risk could also impact access to capital, as lenders and investors may reassess the risk profiles of healthcare providers.
Conversely, a narrow interpretation could offer some relief, but uncertainty remains a significant factor until the full implications are understood and implemented. For example, a ruling that clarifies the standard of knowledge required for liability could significantly alter the risk profile for smaller providers with less robust compliance programs.
Effects on Billing Practices and Compliance Programs
Regardless of the specific outcome, healthcare providers will likely need to review and revise their billing practices and compliance programs. This might involve strengthening internal controls, enhancing documentation procedures, and investing in more sophisticated compliance technology. Providers might also need to reassess their relationships with billing companies and other third-party vendors to ensure compliance. For instance, hospitals may need to increase staff training on proper coding and billing procedures, potentially leading to increased operational costs.
The need for meticulous documentation and robust internal audits will become paramount, requiring a shift towards more stringent and proactive compliance strategies.
Potential Financial Implications for Healthcare Providers
The financial implications could be substantial. Increased legal fees associated with defending against FCA claims, potential penalties for violations, and the costs of implementing enhanced compliance programs could significantly strain budgets, particularly for smaller or financially vulnerable providers. A large penalty could cripple a small clinic, while a major hospital system might absorb the cost but experience a decrease in profitability and potentially impact their ability to invest in infrastructure or new technologies.
The uncertainty surrounding the decision itself introduces financial risk, making long-term planning more challenging. For example, a rural hospital with limited resources might find it difficult to invest in improved compliance systems, leaving them more vulnerable to future legal action.
Adaptation Strategies for Healthcare Providers, Ahip and aha join forces file amicus brief in false claims act scotus case
Healthcare providers will need to adapt proactively to mitigate potential risks. This includes bolstering their compliance programs, conducting thorough internal audits, and investing in training for staff. Engaging legal counsel specialized in healthcare law and the FCA will be crucial for navigating the complexities of the post-decision landscape. Furthermore, strengthening relationships with government agencies and fostering open communication about billing practices can contribute to a more favorable outcome in potential audits or investigations.
Hospitals and physician groups might consider forming collaborative compliance initiatives to share best practices and reduce individual risk. This proactive approach is crucial for maintaining financial stability and ensuring continued operational efficiency.
Impact on Different Types of Healthcare Providers
| Provider Type | Size | Specialization | Potential Impact |
|---|---|---|---|
| Hospital | Large | General | Moderate impact; likely to absorb costs but experience reduced profitability. |
| Hospital | Small | Rural | High impact; potential for significant financial strain and reduced access to capital. |
| Physician Group | Large | Specialty (e.g., Cardiology) | Moderate impact; significant investment in compliance updates needed. |
| Clinic | Small | Primary Care | High impact; potential for closure due to financial burdens from penalties and compliance costs. |
Implications for Patients and Consumers: Ahip And Aha Join Forces File Amicus Brief In False Claims Act Scotus Case
The Supreme Court’s decision in this False Claims Act case, heavily influenced by the joint amicus brief filed by AHIP and AHA, will have far-reaching consequences for patients and consumers across the healthcare landscape. The outcome will significantly shape access to care, influence healthcare costs, and potentially alter the quality of services received. Understanding these potential impacts is crucial for individuals navigating the complexities of the healthcare system.The core issue revolves around the interpretation of the False Claims Act and its implications for healthcare providers’ billing practices.
A ruling favoring stricter interpretations could lead to significant changes in how providers operate, ultimately impacting patients in various ways.
Patient Access to Care
A stricter interpretation of the False Claims Act might lead some providers, particularly those with thinner margins, to limit the services they offer or to restrict patient access to certain treatments. Fear of legal repercussions could incentivize providers to be more selective about the patients they accept, potentially leading to longer wait times for appointments, reduced availability of specialists, and difficulties accessing necessary care, especially for vulnerable populations.
For example, a rural hospital facing increased scrutiny might curtail its services, leaving residents with fewer options for care.
Healthcare Costs for Patients and Consumers
The ruling could also affect patient costs. If providers face increased legal and administrative burdens associated with stricter compliance requirements, they may pass these costs onto patients through higher premiums, co-pays, and deductibles. Increased litigation costs could also drive up insurance premiums for everyone. This could make healthcare unaffordable for many, especially those with limited incomes or those lacking comprehensive insurance coverage.
Imagine a scenario where a hospital, facing expensive legal battles, increases its prices for routine procedures, making it harder for families to afford necessary medical care.
Quality of Healthcare Services
While not directly impacting quality, the increased administrative burden and fear of legal action could indirectly affect the quality of care. Providers might divert resources from patient care to compliance efforts, leading to less time spent with patients, reduced opportunities for preventative care, and potentially a decline in the overall quality of services. For instance, a clinic might prioritize paperwork over patient interaction, leading to missed diagnoses or inadequate treatment plans.
Examples of Patient Impact
The ruling could manifest in various ways for patients. A patient might experience longer wait times for specialist appointments, face difficulties accessing certain treatments due to provider limitations, or see their insurance premiums rise significantly. They might also encounter more stringent documentation requirements or increased scrutiny during their visits. A patient needing a specialized surgery might find fewer providers willing to perform the procedure due to the increased legal risks.
The AHIP and AHA teaming up for that Supreme Court amicus brief on the False Claims Act case got me thinking – healthcare’s a huge battleground. It’s crucial to understand the impact of preventable conditions, like stroke, especially considering factors like high blood pressure and age, which are discussed in detail on this informative site about risk factors that make stroke more dangerous.
This knowledge is vital, because preventing these conditions could significantly reduce the kinds of healthcare fraud the AHIP and AHA are fighting against.
Potential Scenarios and Their Impact on Patient Care
The following scenarios illustrate potential outcomes of the Supreme Court’s decision:
- Scenario: Increased scrutiny of billing practices leads to a reduction in the number of providers offering certain services. Impact: Patients experience longer wait times and reduced access to care, particularly in underserved areas.
- Scenario: Providers increase prices to offset increased legal and administrative costs. Impact: Patients face higher out-of-pocket expenses, making healthcare less affordable.
- Scenario: Providers prioritize compliance over patient care, leading to reduced time spent with patients. Impact: Patients receive less personalized attention, potentially resulting in misdiagnosis or inadequate treatment.
- Scenario: Providers become more risk-averse, leading to a decrease in the availability of innovative or experimental treatments. Impact: Patients with complex conditions may have fewer treatment options.
The Role of AHIP and AHA in Healthcare Policy
The American Hospital Association (AHA) and the America’s Health Insurance Plans (AHIP) are two powerful lobbying groups that significantly shape healthcare policy in the United States. Their combined influence stems from representing a vast network of hospitals and health insurance providers, respectively, giving them considerable weight in legislative and judicial processes. Understanding their roles, past actions, and the implications of their joint involvement in this Supreme Court case is crucial for comprehending the future trajectory of healthcare in America.AHIP and AHA’s roles and responsibilities encompass advocacy, education, and the development of industry best practices.
AHIP focuses primarily on representing the interests of health insurance companies, advocating for policies that support the industry’s profitability while ensuring access to care. The AHA, conversely, champions the interests of hospitals and health systems, focusing on issues like hospital funding, patient safety, and the overall quality of care. Their involvement in shaping healthcare policy extends to lobbying efforts, participation in regulatory rulemaking, and the initiation of legal challenges to policies they deem unfavorable.
AHIP and AHA’s Past Involvement in Legal Cases
Both organizations have a long history of participating in significant legal cases impacting healthcare. AHIP has frequently been involved in litigation concerning the Affordable Care Act (ACA), often arguing for interpretations that favor the interests of insurance providers. The AHA has similarly engaged in legal battles related to Medicare and Medicaid reimbursement rates, advocating for policies that ensure adequate funding for hospitals.
Their past actions demonstrate a willingness to utilize legal channels to advance their policy agendas. For example, AHIP actively participated in cases challenging provisions of the ACA related to insurance mandates and market regulations. The AHA, on the other hand, has been involved in litigation concerning the adequacy of Medicare and Medicaid reimbursement rates, arguing that insufficient payments threaten hospital solvency and the ability to provide quality care.
Significance of Joint Participation in this SCOTUS Case
The joint participation of AHIP and AHA in this False Claims Act case is highly significant. It signals a convergence of interests between two organizations that often find themselves on opposing sides of policy debates. Their united front suggests that the issue at hand—the interpretation of [Specific aspect of the False Claims Act relevant to the case]—has potentially far-reaching consequences for both the insurance industry and hospitals.
This unprecedented collaboration underscores the seriousness of the potential ramifications of the court’s decision.
Broader Implications of AHIP and AHA’s Actions on Healthcare Policy
The actions of AHIP and AHA in this case will likely set a precedent for future healthcare policy debates. Their joint amicus brief demonstrates a willingness to collaborate on issues of mutual concern, potentially influencing future legislative and regulatory efforts. The outcome of this case could significantly impact how healthcare providers and insurers interact, potentially altering reimbursement models, risk allocation, and the overall structure of the healthcare system.
The AHIP and AHA teaming up for that Amicus brief in the False Claims Act Supreme Court case got me thinking about healthcare spending. It’s a huge issue, and the news that Kaiser Permanente just scrapped a $500 million Seattle bed tower kaiser permanente nixes 500m seattle bed tower capital spending really highlights the financial pressures facing the industry.
This decision underscores the importance of the AHIP and AHA’s efforts to clarify the legal landscape surrounding healthcare reimbursements.
The court’s decision will undoubtedly shape future legal strategies and policy debates in the healthcare sector.
Timeline of AHIP and AHA Involvement in Significant Healthcare Policy Debates
This timeline illustrates key moments in AHIP and AHA’s involvement in shaping healthcare policy:
The following timeline provides a simplified overview, focusing on major legislative and legal events. It does not encompass every policy debate or legal action in which either organization has participated.
| Year | Event | AHIP Involvement | AHA Involvement |
|---|---|---|---|
| 2010 | Passage of the Affordable Care Act | Significant lobbying efforts; subsequent legal challenges to specific provisions. | Active lobbying; engagement in subsequent legal challenges regarding hospital funding and reimbursement. |
| 2012-2017 | Various legal challenges to the ACA | Active participation in multiple lawsuits. | Active participation in multiple lawsuits. |
| 2017-Present | Ongoing debates regarding healthcare reform | Continued lobbying and advocacy efforts. | Continued lobbying and advocacy efforts. |
| [Year of Current SCOTUS Case] | Current SCOTUS Case | Joint amicus brief with AHA. | Joint amicus brief with AHIP. |
Outcome Summary
The AHIP and AHA’s amicus brief in this False Claims Act Supreme Court case is more than just a legal filing; it’s a significant intervention in the ongoing debate about healthcare costs, access, and accountability. The outcome will undoubtedly have far-reaching consequences, influencing how hospitals operate, how doctors bill, and ultimately, the quality and affordability of care for all of us.
It’s a situation worth watching closely, and we’ll be here to keep you updated on the developments.
Popular Questions
What is the False Claims Act?
The False Claims Act is a federal law that allows the government to recover money from individuals or entities that defraud it. In healthcare, this often involves allegations of fraudulent billing practices.
Why did AHIP and AHA file a joint brief?
They likely felt the case had significant implications for their members and the broader healthcare industry, and a united front would strengthen their arguments.
What are the potential consequences of the Supreme Court’s decision?
The decision could significantly impact hospital reimbursement, billing practices, and potentially patient access to care depending on the ruling. It could also lead to increased litigation.
How can I stay updated on this case?
Follow reputable news sources covering healthcare law and Supreme Court decisions. You can also check the websites of AHIP and AHA for updates.



