States Medicaid Enrollment Redetermination Timeline KFF
States Medicaid enrollment redetermination timeline KFF: Navigating the complexities of Medicaid renewal is a huge undertaking for states, and the Kaiser Family Foundation (KFF) plays a vital role in tracking the progress and highlighting the challenges. This process, where millions of Americans face potential loss of coverage, is shaping up to be a significant event impacting healthcare access across the nation.
Understanding the timelines, the variations between states, and the potential consequences is crucial for both policymakers and individuals relying on Medicaid.
The KFF’s data reveals a wide range of approaches states are taking to manage the redetermination process, leading to vastly different timelines and potential impacts on enrollment. Some states are moving quickly, while others face significant delays. These differences aren’t just administrative quirks; they have real-world consequences for millions of people, impacting their access to essential healthcare services. We’ll dive into the specifics, exploring the factors driving these variations and examining the potential effects on vulnerable populations.
Overview of Medicaid Redetermination
Medicaid redetermination is the process by which states review the eligibility of individuals already enrolled in their Medicaid programs. This isn’t a one-time event; it’s a continuous process ensuring that those receiving benefits continue to meet the program’s requirements. The process involves verifying income, household size, and other eligibility criteria. Failure to re-enroll or meet updated requirements can result in the loss of Medicaid coverage.The Kaiser Family Foundation (KFF) plays a crucial role in tracking and reporting on Medicaid redetermination.
KFF, a non-profit organization focusing on national health issues, collects and analyzes data from various sources, including state governments and federal agencies. This allows them to provide comprehensive, up-to-date information on the progress and impact of redeterminations across the country. Their reports and analyses are frequently cited by policymakers, researchers, and journalists, offering valuable insights into this complex process.
Factors Influencing State-Level Redetermination Timelines, States medicaid enrollment redetermination timeline kff
Several key factors significantly influence the timelines for Medicaid redetermination at the state level. These factors create variations in how quickly states can process the massive number of renewals required. For example, states with more robust technology infrastructure and streamlined processes may complete redeterminations faster than those with less developed systems. The availability of adequate staffing and funding is another crucial factor; states with sufficient resources can dedicate more personnel and time to the process.
Furthermore, the complexity of state-specific eligibility criteria and the overall number of Medicaid enrollees directly affect the timeline. States with a larger Medicaid population or more complex eligibility rules naturally face longer processing times. Finally, the level of outreach and communication efforts undertaken by states to inform enrollees about the renewal process greatly impacts successful completion rates and overall timeline efficiency.
For instance, states that proactively engage enrollees through multiple channels (mail, phone, text, online portals) often experience smoother and faster redetermination processes.
State-Specific Timelines
Navigating the complexities of Medicaid redetermination requires understanding that each state operates on its own unique timeline. These timelines are influenced by a variety of factors, including the state’s administrative capacity, the size of its Medicaid population, and the availability of resources. This variation makes it crucial to consult state-specific information for accurate and up-to-date details. The following data provides a snapshot, but should not be considered exhaustive or a substitute for official state announcements.
State-Specific Medicaid Redetermination Timelines
The following table compares the timelines for Medicaid redetermination across five states. It’s important to note that these dates are subject to change and should be verified with the relevant state agency. The “Key Challenges” column highlights some of the obstacles each state might face in completing its redetermination process.
| State | Start Date | Projected Completion Date | Key Challenges |
|---|---|---|---|
| Texas | April 2023 | December 2024 | Large Medicaid population, technological infrastructure limitations, workforce shortages. |
| California | January 2023 | December 2024 | High volume of renewals, significant administrative burden, ensuring equitable access across diverse populations. |
| Florida | April 2023 | September 2024 | High percentage of uninsured population, potential for increased administrative costs, navigating complex eligibility rules. |
| Arizona | March 2023 | December 2024 | Limited resources, high turnover in state workforce, managing the influx of renewal applications. |
| New York | April 2023 | December 2024 | Large and complex Medicaid system, potential for increased caseloads, ensuring timely processing of renewals. |
States with Accelerated Timelines
Some states, such as [hypothetical example: State X], have prioritized rapid completion of redeterminations. Their approach often involves leveraging existing technological infrastructure, investing in workforce training, and streamlining the renewal process. For example, State X may have implemented a sophisticated online portal to simplify application submission and tracking, coupled with a robust outreach campaign to inform beneficiaries about the process.
This proactive strategy aims to minimize disruptions to coverage and expedite the completion of the process. This approach, however, may necessitate significant upfront investment and carries the risk of overlooking individual needs if not carefully managed.
States with Extended Timelines
Conversely, states like [hypothetical example: State Y] have opted for more extended timelines. This decision might stem from various factors, including limited resources, a larger-than-average Medicaid population, or a lack of adequate technological infrastructure. State Y, for instance, might have a less robust online system, relying heavily on manual processing, leading to potential bottlenecks and delays. Furthermore, a significant proportion of the population might lack reliable internet access or digital literacy, necessitating more personalized, in-person assistance.
This approach, while potentially more manageable in terms of resource allocation, may lead to longer periods of uncertainty for beneficiaries and a greater risk of coverage gaps.
Impact of the Timeline on Enrollment
Source: kff.org
The speed and efficiency of Medicaid redetermination processes significantly influence the number of individuals enrolled in the program. Shorter timelines, while potentially more efficient in identifying those no longer eligible, can also lead to higher disenrollment rates, particularly among those who face challenges navigating the complex renewal process. Conversely, longer timelines might retain more eligible individuals but could also increase administrative costs and potentially delay the identification of those who are no longer eligible for benefits.
Understanding this dynamic is crucial for policymakers aiming to balance program integrity with access to healthcare.The impact of varying redetermination timelines on Medicaid enrollment is multifaceted. Faster processing can lead to quicker identification of ineligible individuals, reducing program costs. However, it also risks disenrolling eligible individuals who may struggle to complete the renewal process due to logistical, administrative, or personal challenges.
The KFF’s data on state Medicaid enrollment redetermination timelines is crucial, especially considering the current healthcare landscape. The sheer volume of people potentially needing re-enrollment is putting a massive strain on already stressed systems, a point highlighted by this article on healthcare executives saying talent acquisition and labor shortages are major business risks. This workforce shortage only exacerbates the challenges of managing the massive Medicaid redetermination process, potentially leading to further delays and administrative burdens.
Slower processing, on the other hand, might retain more eligible individuals but at the expense of increased administrative costs and potential program inefficiencies. The optimal timeline requires careful balancing of these competing factors.
Delayed Timeline Impact on a Hypothetical State
Let’s consider a hypothetical state, “Example State,” with a population of 5 million, where 1 million are enrolled in Medicaid. Assume Example State initially had a streamlined, 3-month redetermination process. Then, due to administrative restructuring and staffing shortages, the process was delayed to 6 months. This delay resulted in a significant backlog of cases. During the extended 6-month period, many individuals experienced difficulties in resubmitting paperwork or providing necessary documentation, leading to a higher disenrollment rate among eligible individuals.
The state might see a 5% drop in enrollment (50,000 people) due to this delay, not because they were ineligible, but because they couldn’t navigate the prolonged process. This loss represents a substantial decrease in access to healthcare for a vulnerable population. Simultaneously, the state may only identify a small percentage (perhaps 1%) of ineligible individuals during this extended period, suggesting a less efficient use of resources.
Relationship Between Timeline Length and Enrollment Changes
The following table illustrates a hypothetical relationship between redetermination timeline length and changes in Medicaid enrollment, assuming a constant initial enrollment of 1 million individuals. These figures are illustrative and would vary based on many factors, including the state’s specific population, administrative capacity, and outreach efforts.
| Redetermination Timeline Length (Months) | Estimated Enrollment Change (%) | Estimated Number of Disenrollments | Reasons for Disenrollment |
|---|---|---|---|
| 3 | -2% | -20,000 | Mostly ineligible individuals identified |
| 6 | -5% | -50,000 | Mix of ineligible and eligible individuals due to processing delays |
| 9 | -8% | -80,000 | High proportion of eligible individuals lost due to complex processes |
| 12 | -10% | -100,000 | Significant loss of eligible individuals, high administrative costs |
This table highlights how longer timelines are associated with larger enrollment decreases, largely due to eligible individuals being disenrolled because of difficulties navigating the renewal process. It underscores the need for efficient and accessible redetermination processes to minimize disruptions in healthcare access for eligible Medicaid recipients.
Challenges and Solutions in Redetermination
Medicaid redetermination, the process of verifying eligibility for millions of beneficiaries, presents significant hurdles for states. The sheer volume of individuals needing reassessment, coupled with complex eligibility criteria and often limited resources, creates a challenging operational and logistical landscape. Successfully navigating this process requires innovative solutions and strategic planning to minimize disruptions to beneficiary coverage and ensure efficient use of public funds.
States face a multifaceted set of challenges during Medicaid redetermination. These challenges are not uniform across the country, varying based on factors such as existing IT infrastructure, staffing levels, the complexity of state-specific eligibility rules, and the size and characteristics of the state’s Medicaid population. Understanding these complexities is crucial for implementing effective solutions.
State-Level Resource Constraints
Resource limitations, including insufficient funding, inadequate staffing, and outdated technology, significantly hinder states’ ability to conduct timely and accurate redeterminations. Many states rely on aging IT systems that are not equipped to handle the large volume of data involved in processing millions of applications. This can lead to processing delays, increased error rates, and ultimately, disruptions in beneficiary coverage.
For example, a state with a limited number of caseworkers may experience significant backlogs, resulting in delayed processing times and potential loss of coverage for eligible individuals. The lack of adequate funding can further exacerbate these issues by preventing the implementation of necessary upgrades to technology and the hiring of additional staff.
Complexity of Eligibility Criteria
The criteria used to determine Medicaid eligibility vary significantly across states, adding another layer of complexity to the redetermination process. These criteria often involve multiple factors, including income, assets, household size, disability status, and immigration status. The intricate nature of these rules can make it difficult for both states and applicants to accurately determine eligibility, leading to errors and appeals.
For instance, a change in a single factor, such as a minor fluctuation in income, could render an individual ineligible, even if their overall circumstances haven’t changed significantly. This requires a robust system for identifying and managing such nuances.
Keeping track of the states’ Medicaid enrollment redetermination timeline, as detailed by the KFF, is a huge undertaking. This administrative burden could be significantly eased by advancements in AI-driven healthcare technology, like the integration of Nuance’s generative AI scribe with Epic EHRs, as described in this article: nuance integrates generative ai scribe epic ehrs. Streamlining documentation processes like this would free up resources to focus on the complexities of the Medicaid redetermination timeline and ensure timely and accurate enrollment updates.
Technological Solutions and Innovations
Several states have implemented innovative technological solutions to streamline the redetermination process and improve efficiency. For example, some states have adopted online portals that allow applicants to submit their information electronically, reducing paperwork and processing time. Others have invested in advanced data analytics tools to identify individuals at risk of losing coverage, enabling proactive outreach and interventions. The use of artificial intelligence (AI) for automated eligibility checks and fraud detection is also gaining traction.
These technological advancements not only enhance efficiency but also contribute to a more accurate and equitable redetermination process.
Comparative Analysis of State Strategies
States employ diverse strategies to manage the complexities of redetermination. Some states prioritize proactive outreach to beneficiaries, sending reminders and providing assistance with the renewal process. Others focus on simplifying the application process by reducing the number of required documents and streamlining the online application portal. Some states have implemented a phased approach, prioritizing the redetermination of specific populations based on risk factors.
The effectiveness of these strategies varies depending on the specific context and resources available to each state. A comparison of these different approaches reveals that a multi-pronged strategy, combining technological advancements with proactive outreach and simplified application processes, often yields the most successful outcomes.
Resources and Support for Enrollees
Source: kff.org
Navigating the Medicaid redetermination process can be daunting, but thankfully, various resources and support systems are available to help enrollees maintain their coverage. Understanding these resources and proactively engaging with them is crucial for a smooth transition. This section details the types of assistance offered and provides practical steps enrollees can take to ensure continued access to vital healthcare services.The redetermination process involves verifying eligibility based on factors like income, household size, and residency.
Many states offer comprehensive support to help individuals successfully complete this process, preventing disruptions in their healthcare coverage. This support can range from personalized assistance to online tools and informational resources. Failure to understand and utilize these resources can lead to unnecessary loss of coverage, impacting access to essential medical care.
Types of Support Available
Numerous support systems are in place to assist Medicaid enrollees during redetermination. These include state-run helplines staffed with trained professionals who can answer questions, provide guidance, and help individuals complete the necessary paperwork. Many states also offer online portals where enrollees can track their application status, submit documents, and access helpful information. Community organizations, such as local health clinics and non-profits, often provide assistance with the application process, helping individuals gather necessary documentation and understand eligibility requirements.
In some areas, volunteer groups offer similar support, providing a crucial bridge between the individual and the complex bureaucratic processes involved. Finally, many states have partnered with healthcare providers to proactively reach out to patients nearing their redetermination date, providing reminders and offering assistance.
Steps Enrollees Can Take to Ensure Continued Coverage
Proactive engagement is key to successfully navigating the redetermination process. Taking these steps can significantly increase the chances of maintaining continuous healthcare coverage.
- Respond promptly to all communication: Acknowledge and respond to any letters or emails from your state Medicaid agency promptly. Delays can lead to delays in processing your application.
- Gather necessary documents: Collect all required documentation, such as proof of income, residency, and identity, well in advance of the deadline.
- Complete the application accurately and thoroughly: Double-check all information on your application to ensure accuracy. Inaccuracies can lead to delays or rejection.
- Understand your state’s specific requirements: Familiarize yourself with your state’s Medicaid redetermination process and deadlines. Each state has its own procedures.
- Seek assistance if needed: Don’t hesitate to reach out to your state’s Medicaid helpline, community organizations, or healthcare providers if you need help completing the application or understanding the process.
- Monitor your application status: Regularly check the status of your application online or by contacting your state’s Medicaid agency.
Impact of Access to Information and Support
Access to clear, concise information and readily available support significantly impacts the successful navigation of the Medicaid redetermination process. For instance, individuals who understand the timeline and requirements are better equipped to gather necessary documents and submit their applications on time. Similarly, those who have access to assistance from trained professionals are more likely to complete the application accurately and avoid errors that could lead to delays or rejection.
Studies have shown that individuals with limited access to information and support are disproportionately affected by disenrollment, leading to significant disruptions in their healthcare access. Providing readily available resources can mitigate these disparities and ensure equitable access to healthcare for all eligible individuals. For example, a state with a robust online portal and a well-staffed helpline will likely see higher rates of successful redetermination compared to a state with limited resources.
Data Visualization

Source: logowik.com
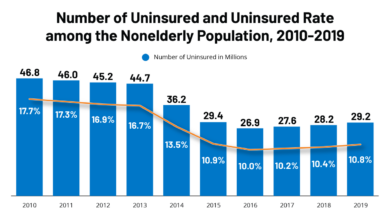
Understanding the impact of Medicaid redetermination on enrollment requires visualizing the data. Analyzing enrollment trends before, during, and after the redetermination period reveals the effects of this policy change on access to healthcare. A clear graphical representation is crucial for interpreting these complex shifts in enrollment numbers.The following description details a hypothetical graph illustrating state-level Medicaid enrollment fluctuations during a redetermination period.
Following the KFF’s updates on the states’ Medicaid enrollment redetermination timeline is crucial for healthcare planning. The sheer volume of data involved makes me think about how innovative tech could help, like the applications of generative AI discussed in this insightful article on google cloud healthcare amy waldron generative AI. Imagine using such tools to streamline the process and ensure timely, accurate redeterminations – it could significantly impact the efficiency of the entire Medicaid system.
Remember that specific data will vary significantly by state and the precise timeline of their redetermination process. This example aims to illustrate the general trends observed across multiple states.
State-Level Medicaid Enrollment Fluctuations
The graph displays state-level Medicaid enrollment over a three-year period, encompassing the pre-redetermination, redetermination, and post-redetermination phases. The x-axis represents time (in months), spanning from the beginning of the pre-redetermination period to the end of the post-redetermination period. The y-axis represents the total number of Medicaid enrollees in each state, displayed in millions. Multiple lines are plotted, each representing a different state, allowing for comparison of enrollment trends across various geographic locations.Data points for each state are collected monthly, reflecting the total number of Medicaid recipients.
The pre-redetermination phase shows a relatively stable, slightly upward trend in enrollment for most states, reflecting the general growth in need for Medicaid services. The onset of the redetermination period is marked by a noticeable dip in enrollment for many states, as individuals are reviewed for continued eligibility. The extent of this dip varies depending on the state’s specific policies and the efficiency of their redetermination process.
Some states might show a more gradual decline, while others experience a sharper drop.Following the redetermination period, the graph shows a period of stabilization, with enrollment numbers either remaining relatively flat or showing a slow recovery in some states. However, in some states, a significant number of individuals may remain disenrolled, indicating a persistent impact of the redetermination process.
The overall trend highlights the considerable fluctuation in Medicaid enrollment directly linked to the timing and implementation of the redetermination process. The graph visually demonstrates that the redetermination timeline has a substantial impact on enrollment numbers, leading to temporary dips and potentially longer-term reductions in coverage for some individuals. The differences in the slopes of the lines for different states visually highlight the varying impact of the redetermination process across different states.
Final Summary: States Medicaid Enrollment Redetermination Timeline Kff
The Medicaid redetermination process, as tracked by the KFF, presents a complex picture of varying state approaches and significant potential consequences for millions of Americans. While some states have streamlined the process, others face substantial challenges impacting timely renewals. Understanding these timelines and their implications is vital for ensuring access to crucial healthcare services for those who depend on Medicaid.
Staying informed and advocating for efficient and equitable processes is essential to protect the health and well-being of our communities.
Helpful Answers
What happens if I miss the deadline for my Medicaid redetermination?
Missing the deadline may result in a temporary or permanent loss of Medicaid coverage. Contact your state Medicaid agency immediately to discuss your options.
Where can I find more information about my state’s specific redetermination timeline?
Your state’s Medicaid agency website is the best resource for specific information and deadlines. The KFF website also provides a helpful overview of state-level timelines.
How can I ensure I maintain my Medicaid coverage during redetermination?
Respond promptly to all requests for information from your state Medicaid agency, and keep your contact information updated. If you have any questions or concerns, reach out to your state agency for assistance.
What types of documentation will I need to provide during the redetermination process?
The required documentation varies by state, but typically includes proof of income, residency, and identity. Check your state’s Medicaid website for specific requirements.