COVID Pandemic Telehealth Flexibilities Expire
COVID pandemic public health emergency telehealth flexibilities expire – it’s a headline that’s been looming for months, and now it’s here. The end of expanded telehealth access means a potential shift back to traditional in-person healthcare, raising concerns about accessibility, affordability, and overall patient care. This change impacts everyone, from patients with chronic conditions relying on virtual check-ins to healthcare providers adapting to new reimbursement models.
Let’s dive into what this means for the future of healthcare.
The impact of this shift is multifaceted. We’ll explore the potential financial strain on patients and providers, examine the regulatory landscape, and hear directly from patients about their experiences with telehealth during the pandemic and beyond. We’ll also look at the innovative technological advancements that might help bridge the gap left by the expiring flexibilities, and consider the implications for public health in the long term.
Get ready for a comprehensive look at this crucial moment in healthcare history.
Impact of Telehealth Flexibilities Expiration
The expiration of COVID-19 telehealth flexibilities marks a significant turning point in healthcare access. While telehealth exploded in popularity during the pandemic, offering convenient and often safer alternatives to in-person visits, its future is now uncertain as many of the regulatory allowances that fueled its growth are rescinded. This shift will undoubtedly impact various aspects of healthcare delivery and patient access, potentially exacerbating existing health disparities.The potential effects of this expiration are multifaceted and far-reaching.
Reduced access to care, particularly for rural or underserved populations, is a major concern. Many patients who relied on telehealth for routine check-ups, mental health services, and chronic disease management may find themselves facing significant barriers to continuing this care. This is especially true for those with limited transportation options, mobility challenges, or those who live in areas with a shortage of healthcare providers.
The convenience and affordability of telehealth, which often resulted in lower overall healthcare costs for patients, are also at risk.
Changes in Healthcare Utilization Patterns
The shift away from telehealth is likely to lead to a decrease in overall healthcare utilization, at least initially. Some patients may be hesitant to return to in-person visits due to concerns about infection or simply because they found telehealth more convenient. However, other patients who need more hands-on care, such as those requiring physical examinations or complex procedures, will likely still seek in-person care.
This could lead to increased demand for in-person appointments, potentially resulting in longer wait times and increased pressure on existing healthcare systems. For example, we might see a surge in appointments for routine check-ups and preventative care, as patients who delayed these visits during the pandemic try to catch up. Conversely, there might be a decline in the use of telehealth for less urgent matters.
Comparison of Pre- and Post-Pandemic Telehealth Landscapes
Before the pandemic, telehealth was a niche service, largely limited to specific situations like remote monitoring of chronic conditions or specialist consultations. Reimbursement rates were often low, and many providers lacked the infrastructure or training to offer telehealth services effectively. The pandemic dramatically changed this landscape. Regulatory changes allowed for broader telehealth adoption, and increased reimbursement rates incentivized providers to invest in the necessary technology and training.
Patients quickly embraced the convenience and accessibility of telehealth, leading to a significant increase in its use. The post-pandemic landscape, however, represents a regression towards a more restricted model. While telehealth will likely remain a part of healthcare delivery, its scope and accessibility will likely be diminished, unless further legislative action is taken to ensure continued expansion.
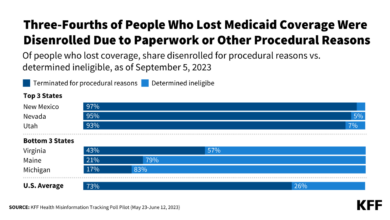
Disparities in Access to Care Created by Expiration
The expiration of telehealth flexibilities is likely to disproportionately affect vulnerable populations. Individuals in rural areas, low-income communities, and those with disabilities often face significant barriers to accessing healthcare even under normal circumstances. The convenience and accessibility of telehealth helped to mitigate some of these barriers, but its reduced availability will likely exacerbate existing disparities. For example, patients who rely on public transportation may find it difficult or impossible to attend in-person appointments, while those with limited digital literacy may struggle to navigate telehealth platforms effectively.
This disparity in access to technology and transportation will likely lead to poorer health outcomes for these vulnerable groups. Consider, for instance, a diabetic patient in a rural area who relied on telehealth for regular blood glucose monitoring and consultations with their endocrinologist. The loss of telehealth access could lead to delays in diagnosis and treatment, potentially resulting in serious complications.
Financial Implications of the Expiration
Source: bmj.com
The end of the COVID-19 public health emergency telehealth flexibilities has significant financial ramifications for both patients and healthcare providers. The increased accessibility and convenience of telehealth during the pandemic masked underlying cost structures, and the return to more traditional models exposes potential financial burdens and necessitates careful consideration of cost-saving strategies.
Patient Financial Burdens from Reduced Telehealth Access
The decreased availability of telehealth will likely lead to increased healthcare costs for many patients. Travel expenses to in-person appointments, including gas, parking, and potentially lost wages, become significant factors. For patients in rural areas or those with mobility limitations, the inability to access telehealth could mean foregoing necessary care altogether, leading to potentially more expensive health issues down the line.
Additionally, the higher cost of in-person visits compared to telehealth appointments will directly impact patients’ out-of-pocket expenses, particularly those with high deductibles or limited insurance coverage. For example, a patient with a high deductible might find that a $50 telehealth visit becomes a $200 in-person visit, significantly impacting their budget.
Impact on Healthcare Providers’ Revenue Streams
The shift away from telehealth will also impact healthcare providers’ revenue streams. While some in-person visits will naturally command higher fees, reimbursement rates for telehealth services often differed from those for in-person visits, sometimes favorably for providers. The return to pre-pandemic reimbursement models may lead to reduced revenue, particularly for specialists who relied heavily on telehealth for patient access.
This could lead to decreased provider income, potential staff reductions, or limitations in the services offered, particularly in areas where telehealth had been a significant driver of access. For instance, a rural clinic heavily reliant on telehealth for consultations might experience a drop in revenue due to lower reimbursement for in-person visits, impacting their ability to maintain staffing levels.
So, the COVID-19 pandemic public health emergency telehealth flexibilities are expiring, leaving many wondering what’s next for virtual care. This shift makes the timing of the CMS launching a new primary care Medicare model ACO, as detailed in this article cms launches primary care medicare model aco , particularly interesting. It’ll be crucial to see how this new model integrates telehealth going forward, especially given the recent changes to remote care access following the end of the public health emergency.
Cost-Saving Measures for Patients and Providers
Despite the challenges, there are potential cost-saving measures for both patients and providers. For patients, exploring options like telehealth services offered by larger health systems or negotiating payment plans with providers can help manage costs. For providers, streamlining administrative processes, optimizing staffing models, and exploring value-based care models can help offset revenue losses and maintain financial stability. Negotiating lower rates with telehealth platforms or exploring bundled payment models could also prove beneficial.
Furthermore, promoting preventative care and encouraging patients to utilize telehealth for routine check-ups or follow-ups could help minimize the need for expensive in-person visits for minor issues.
Comparison of In-Person vs. Telehealth Visit Costs, Covid pandemic public health emergency telehealth flexibilities expire
| Medical Specialty | In-Person Visit Cost (Estimate) | Telehealth Visit Cost (Estimate) | Cost Difference |
|---|---|---|---|
| Primary Care | $150 – $250 | $75 – $150 | $75 – $100 |
| Cardiology | $200 – $350 | $100 – $200 | $100 – $150 |
| Mental Health | $175 – $300 | $100 – $175 | $75 – $125 |
| Dermatology | $250 – $400 | $125 – $200 | $125 – $200 |
Regulatory and Policy Responses to Expiration
The expiration of COVID-19 pandemic telehealth flexibilities has triggered a wave of regulatory and policy responses at both the federal and state levels. These responses aim to balance the desire to maintain expanded telehealth access with the need to ensure program sustainability, appropriate oversight, and equitable access for all patients. The resulting landscape is complex, with significant variations across states.The federal government’s role is primarily focused on setting national standards and providing funding for telehealth initiatives.
However, the implementation and specifics of telehealth policies are largely determined at the state level, leading to a patchwork of regulations across the country.
Federal Telehealth Reimbursement and Access Regulations
Following the end of the public health emergency, the Centers for Medicare & Medicaid Services (CMS) has worked to establish permanent telehealth policies. This includes defining covered telehealth services, eligible providers, and patient locations. While some telehealth flexibilities were allowed to lapse, CMS has maintained reimbursement for certain telehealth services that demonstrated efficacy during the pandemic. However, the criteria for reimbursement are stricter than those in place during the emergency, potentially limiting access for some patients and providers.
For instance, the geographic restrictions on telehealth services have become more stringent, requiring patients to reside in rural or underserved areas in many cases. Specific reimbursement rates are also subject to ongoing review and adjustment.
State-Level Telehealth Policies and Best Practices
States have taken diverse approaches to regulating telehealth post-pandemic. Some states have enacted legislation to permanently expand telehealth access, mirroring or exceeding the flexibilities provided during the emergency. These states often have robust telehealth regulatory frameworks that address issues such as licensure, reimbursement rates, and patient privacy. Other states have adopted a more cautious approach, maintaining some telehealth flexibilities on a temporary basis or focusing on specific telehealth applications.
For example, some states have prioritized telehealth for mental health services, while others have concentrated on expanding telehealth access in rural areas. This variability underscores the need for continued monitoring and evaluation of state-level telehealth policies to identify best practices and effective strategies. States like California and New York, with their large and diverse populations, serve as notable examples; their policies, while differing in some aspects, reflect a commitment to integrating telehealth into the long-term healthcare landscape.
Key Policy Changes Since the Start of the Pandemic
The pandemic dramatically accelerated the adoption of telehealth. Prior to 2020, telehealth was a relatively niche area of healthcare. However, the emergency necessitated a rapid expansion of telehealth services, leading to significant policy changes. These changes include temporary waivers of regulations concerning provider licensing, patient location, and types of services covered by insurance. The initial relaxation of these rules allowed for a rapid increase in telehealth utilization, providing access to care for patients who might otherwise have been unable to receive it.
However, as the pandemic waned, these waivers began to expire, necessitating the development of permanent telehealth policies. The shift from temporary, emergency-based policies to more permanent, structured regulations represents a key policy change. This transition involves ongoing negotiations between healthcare providers, insurance companies, and government agencies to determine the long-term sustainability and equitable access to telehealth services. The ongoing discussion regarding the appropriate level of federal versus state regulation remains a crucial element of these policy changes.
Patient Experiences and Perspectives
The end of pandemic-era telehealth flexibilities marks a significant shift for patients who have grown accustomed to the convenience and accessibility of virtual care. Understanding their experiences is crucial to shaping future healthcare policy and ensuring equitable access to care. This section explores patient perspectives, highlighting both the benefits and challenges associated with telehealth, and examining factors influencing satisfaction.
The transition away from expanded telehealth access will undoubtedly impact patients differently. Some will experience a return to potentially inconvenient or inaccessible in-person care, while others may find ways to continue utilizing telehealth where available, albeit perhaps with more limitations. Understanding these varied experiences is key to a smooth transition and to preventing negative health outcomes.
Examples of Patient Experiences with Telehealth
Many patients found telehealth incredibly beneficial during the pandemic. For example, Mrs. Garcia, a 70-year-old with mobility issues, appreciated the ability to receive her routine check-ups from the comfort of her home, eliminating the need for difficult transportation arrangements. Conversely, Mr. Jones, a young professional, valued the time saved by avoiding commutes to appointments, allowing him to maintain his busy work schedule.
However, not all experiences were positive. Ms. Lee, a patient with limited digital literacy, struggled to navigate the telehealth platform, requiring assistance from family members. This highlights the digital divide and the need for equitable access to technology and support.
Challenges and Benefits of Telehealth for Patients
Patients experienced a range of challenges and benefits. Benefits included increased convenience and accessibility, reduced travel time and costs, and improved access to specialists. Challenges included technological difficulties (internet connectivity, device access, digital literacy), concerns about the quality of care, a lack of personal interaction, and difficulties with physical examinations that were impossible to conduct remotely.
Factors Influencing Patient Satisfaction with Telehealth
Several factors influence patient satisfaction. These include the ease of scheduling and access, the quality of the virtual interaction with the provider, the clarity of communication, the effectiveness of the treatment, and the overall convenience and efficiency of the telehealth experience. Patients with chronic conditions might value the regular, remote check-ins more than those with less frequent healthcare needs.
Similarly, patients with limited technological skills may experience lower satisfaction than those comfortable with technology.
Survey on Patient Preferences Regarding In-Person vs. Telehealth Appointments
To gather data on patient preferences, a survey could be designed with the following questions:
The following survey aims to understand your preferences regarding in-person and telehealth appointments. Your honest responses will help shape future healthcare delivery models. All responses will be kept confidential.
| Question | Response Options |
|---|---|
| How often do you typically require medical appointments? | Rarely (less than once a year), Occasionally (1-3 times a year), Frequently (4-12 times a year), Very Frequently (more than 12 times a year) |
| For routine check-ups, would you prefer in-person or telehealth appointments? | In-person, Telehealth, No preference |
| For specialist appointments, would you prefer in-person or telehealth appointments? | In-person, Telehealth, No preference |
| How satisfied were you with the convenience of telehealth appointments during the pandemic (if applicable)? | Very satisfied, Satisfied, Neutral, Dissatisfied, Very dissatisfied |
| What are your primary concerns about telehealth appointments? (Check all that apply) | Technical difficulties, Quality of care concerns, Lack of personal interaction, Difficulty with physical examination, Other (please specify) |
| Do you have reliable internet access at home? | Yes, No |
| How comfortable are you using technology for healthcare purposes? | Very comfortable, Comfortable, Neutral, Uncomfortable, Very uncomfortable |
Technological Advancements and Future of Telehealth: Covid Pandemic Public Health Emergency Telehealth Flexibilities Expire
The COVID-19 pandemic dramatically accelerated the adoption of telehealth, revealing its potential to transform healthcare delivery. While the initial surge was driven by necessity, the future of telehealth hinges on technological innovation that enhances accessibility, effectiveness, and integration into existing healthcare systems. This will not only improve patient care but also reshape the healthcare landscape as a whole.The integration of advanced technologies promises to overcome some of the limitations encountered during the pandemic’s initial telehealth expansion.
Improved bandwidth and network infrastructure, coupled with sophisticated software, are paving the way for a more seamless and reliable telehealth experience.
Remote Patient Monitoring and Wearable Technology
Remote patient monitoring (RPM) is rapidly evolving, using wearable sensors and connected devices to collect vital signs and other health data continuously. This allows for proactive intervention, preventing hospital readmissions and improving patient outcomes. For instance, patients with chronic conditions like heart failure can have their weight, blood pressure, and heart rate monitored remotely, alerting clinicians to potential problems before they escalate.
This proactive approach reduces the burden on hospitals and improves the quality of life for patients. Wearable technology, such as smartwatches and fitness trackers, further expands the scope of RPM, providing valuable data on activity levels, sleep patterns, and other health indicators.
Artificial Intelligence and Machine Learning in Telehealth
AI and machine learning (ML) are poised to revolutionize telehealth by automating tasks, improving diagnostic accuracy, and personalizing treatment plans. AI-powered diagnostic tools can analyze medical images, such as X-rays and CT scans, assisting clinicians in making more accurate diagnoses. ML algorithms can predict patient risks, identify patterns in health data, and personalize treatment recommendations based on individual patient characteristics.
For example, an AI system might analyze a patient’s electronic health record and predict their likelihood of developing a specific condition, enabling proactive interventions.
Enhanced Virtual Reality and Augmented Reality Applications
Virtual reality (VR) and augmented reality (AR) are emerging as powerful tools in telehealth, offering immersive and interactive experiences for both patients and clinicians. VR can be used for virtual therapy sessions, allowing patients to access mental health services remotely in a more engaging environment. AR can overlay digital information onto real-world environments, assisting surgeons with complex procedures or guiding patients through medication administration.
Imagine a surgeon using AR glasses to see a patient’s internal anatomy superimposed on their body during a minimally invasive procedure.
Telehealth Integration Across Healthcare Settings
Telehealth is no longer limited to isolated virtual consultations. Its integration across various healthcare settings is creating a more comprehensive and coordinated approach to care. Hospitals are using telehealth to remotely monitor patients post-discharge, reducing readmissions and improving patient outcomes. Primary care clinics are utilizing telehealth for routine check-ups and follow-up appointments, improving access to care for patients in rural or underserved areas.
Telehealth is also being integrated into specialized care settings, such as oncology and cardiology, allowing patients to receive specialized care without traveling long distances. For instance, a rural oncology patient could receive consultations and treatment planning from a leading cancer center via telehealth, eliminating the need for extensive travel.
Public Health Implications

Source: co.id
The expiration of COVID-19 pandemic telehealth flexibilities presents a significant challenge to public health. The increased access to telehealth during the pandemic demonstrably improved healthcare access, particularly for vulnerable populations. The potential rollback of these flexibilities risks reversing these gains and negatively impacting numerous public health outcomes.The convenient and often cost-effective nature of telehealth significantly improved access to care, especially for individuals in rural or underserved areas, those with mobility issues, or those managing chronic conditions.
A reduction in telehealth access will disproportionately affect these groups, leading to potential delays in diagnosis and treatment, increased hospitalizations, and ultimately, poorer health outcomes.
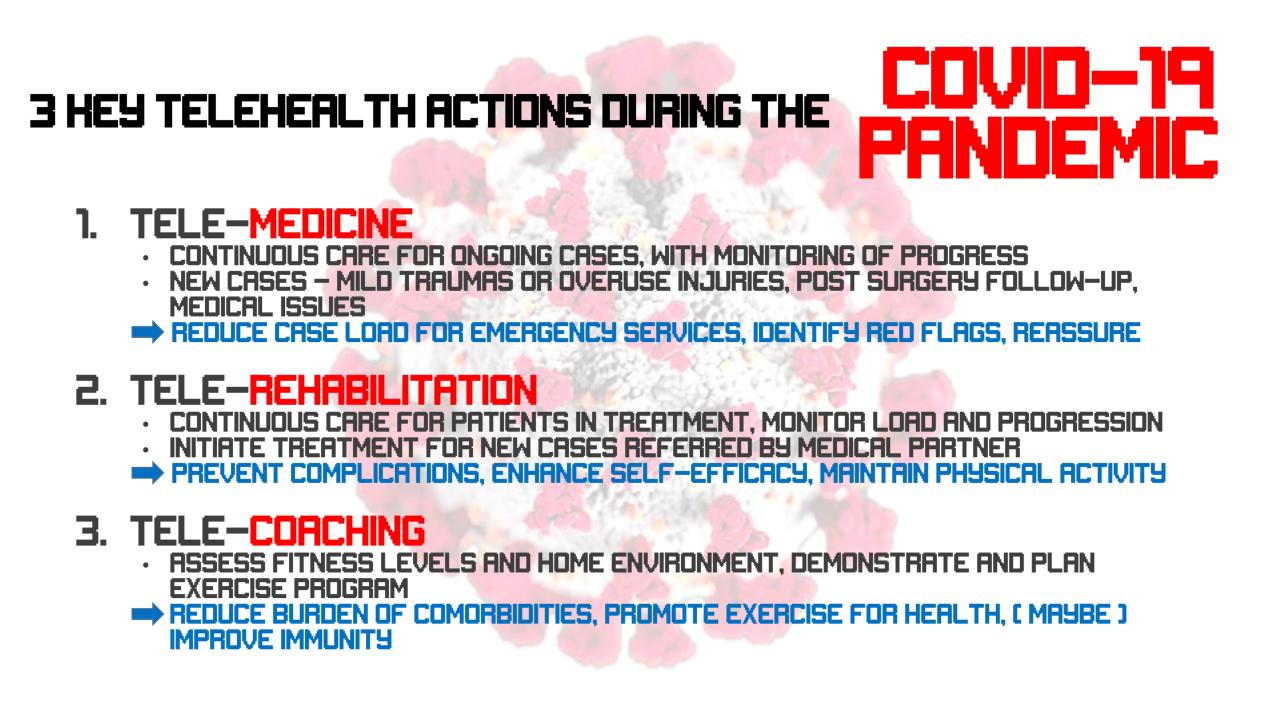
Telehealth’s Role in Chronic Disease Management and Outbreak Prevention
Telehealth played a crucial role in managing chronic diseases during the pandemic. Remote monitoring of vital signs, medication adherence support, and virtual consultations allowed for proactive intervention and improved patient outcomes for conditions like diabetes, hypertension, and heart failure. Furthermore, telehealth facilitated rapid response during outbreaks by enabling early detection, case identification, and contact tracing, reducing the spread of infectious diseases.
The loss of these capabilities will hinder effective chronic disease management and potentially lead to increased morbidity and mortality, along with slower responses to future outbreaks.
Strategies to Mitigate Negative Public Health Consequences
To mitigate the negative impacts of reduced telehealth access, several strategies are crucial. Firstly, policymakers need to advocate for the permanent expansion of telehealth coverage and reimbursement policies. This would ensure continued access for patients regardless of location or socioeconomic status. Secondly, investment in broadband infrastructure is essential to bridge the digital divide and ensure equitable access to telehealth services across all communities.
Thirdly, training and support for healthcare providers in utilizing telehealth technologies are necessary to ensure the effective and safe delivery of care. Finally, public health campaigns promoting telehealth as a viable and beneficial option for healthcare can increase patient adoption and utilization.
Visual Representation of Telehealth Access and Public Health Indicators
Imagine a graph with two axes. The horizontal axis represents the level of telehealth access, ranging from “low” to “high.” The vertical axis represents various public health indicators, including rates of chronic disease hospitalization, emergency room visits for preventable conditions, and the prevalence of uncontrolled chronic diseases. The graph would show a clear downward trend in these negative public health indicators as telehealth access increases.
With the COVID-19 pandemic public health emergency telehealth flexibilities expiring, access to crucial healthcare services might decrease. This is especially worrying considering conditions like stroke, where rapid intervention is vital. Understanding the risk factors that make stroke more dangerous is key to prevention, and timely access to telehealth could be a game-changer in identifying and managing those risks.
The end of these flexibilities could unfortunately impact early stroke detection and treatment.
For example, a point on the graph representing “high” telehealth access would correspond to significantly lower rates of hospitalization for chronic diseases compared to a point representing “low” telehealth access. This visual representation would highlight the strong correlation between increased telehealth access and improved public health outcomes. This positive correlation could be further substantiated by including data points representing specific communities or patient demographics, highlighting the disparities in access and their impact on health outcomes.
For instance, a comparison of rural versus urban populations could showcase how increased telehealth access in rural areas significantly improved health outcomes previously limited by geographical barriers.
The end of the COVID-19 public health emergency means telehealth flexibilities are disappearing, leaving many wondering about access to care. This is especially concerning given recent news that HSHS Prevea is closing some Wisconsin hospitals and health centers, hshs prevea close wisconsin hospitals health centers , potentially impacting telehealth availability even further. The loss of these facilities, coupled with the rollback of telehealth rules, could create serious healthcare access issues for vulnerable populations.
Closure
Source: stanford.edu
The expiration of COVID-19 telehealth flexibilities marks a significant turning point in healthcare. While the convenience and accessibility of telehealth have been undeniably beneficial, the transition back to a more traditional model presents both challenges and opportunities. By understanding the potential financial implications, regulatory changes, and patient perspectives, we can work towards a future where telehealth remains a viable and accessible option for all, regardless of location or socioeconomic status.
The journey towards a sustainable and equitable healthcare system incorporating the best of telehealth is just beginning.
Helpful Answers
What happens to my telehealth appointments now that the flexibilities have expired?
It depends on your insurance provider and the specific telehealth services you’re using. Some services might continue, but others may require in-person visits or may no longer be covered by insurance.
Will my insurance still cover telehealth visits?
Coverage varies widely by insurance plan and state. Contact your insurance provider directly to understand your specific coverage.
What are the alternatives to telehealth if my insurance doesn’t cover it?
Options include seeking out providers who offer sliding-scale fees or finding community health clinics that offer affordable care. You can also explore options like negotiating payment plans with your doctor.
What if I live in a rural area with limited access to in-person healthcare?
Advocating for continued telehealth access in your area is crucial. Contact your state representatives and participate in public forums to express your needs.