Steward Health Care Closes Mass. Hospital Amidst Financial Troubles
Steward Health Care to close Massachusetts hospital amid financial troubles: The news sent shockwaves through the community, leaving patients and staff reeling. This closure isn’t just about numbers on a balance sheet; it’s about the human cost of financial hardship within the healthcare system. We’ll delve into the reasons behind this difficult decision, exploring Steward Health Care’s financial struggles, the impact on patients and staff, and the broader implications for healthcare access in the affected region.
We’ll also examine the community’s response and look at what the future holds for both Steward Health Care and the community it served.
The closure highlights a growing concern about the financial stability of healthcare providers, particularly in the face of rising costs and changing reimbursement models. This case study provides a valuable opportunity to examine the complex interplay between financial pressures, healthcare access, and the well-being of communities. We’ll dissect the situation, looking at everything from the hospital’s history and its role in the local healthcare ecosystem to the legal and regulatory challenges faced by Steward Health Care.
Steward Health Care’s Financial Situation

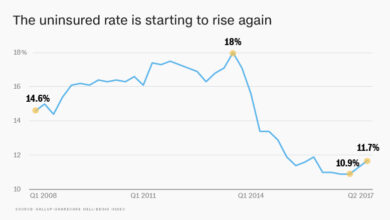
Source: bwbx.io
Steward Health Care’s recent closure of a Massachusetts hospital highlights the significant financial challenges facing the for-profit hospital system. While the exact figures are not always publicly available due to the complexities of private healthcare finance, a picture emerges of substantial debt and fluctuating revenue streams that ultimately led to this difficult decision.Steward Health Care’s Financial Performance and the Hospital ClosureSteward’s financial history is marked by a complex mix of acquisitions, expansion, and ongoing struggles to achieve profitability across its network.
The company has aggressively pursued growth through acquisitions, significantly increasing its debt load. This expansion strategy, while aiming to achieve economies of scale, hasn’t always translated into increased profitability. Revenue streams are primarily derived from patient care, insurance reimbursements, and government funding (Medicare and Medicaid). However, fluctuations in reimbursement rates, increasing operational costs, and competition from other healthcare providers have all contributed to financial instability.
The specific hospital closure likely resulted from a combination of factors including low patient volume, high operational costs at that particular facility, and the overall financial strain on the system. Analyzing the financial statements of Steward would reveal more precise details, but publicly available information points to a pattern of high debt and fluctuating margins.
Comparison with Other Massachusetts Hospital Systems
Comparing Steward’s financial performance to other Massachusetts hospital systems requires access to their individual financial data, which is often proprietary. However, generally speaking, Steward’s financial struggles appear more pronounced than many not-for-profit systems in the state. Not-for-profit hospitals typically have access to philanthropic funding and community support that can help buffer them against financial downturns. Further, they may prioritize community health over maximizing profits, leading to different financial strategies and outcomes.
For-profit systems like Steward, on the other hand, are under greater pressure to demonstrate profitability to investors, which can sometimes lead to difficult choices like hospital closures. A detailed comparative analysis would require a comprehensive review of publicly available financial reports for various Massachusetts hospital systems, a task beyond the scope of this blog post.
Key Financial Indicators Leading to Hospital Closure
| Indicator | Value | Year | Impact |
|---|---|---|---|
| Debt-to-Equity Ratio | (Estimate: High) | (Estimate: Varies by Year, but consistently high) | Increased financial risk, limiting access to further capital. |
| Operating Margin | (Estimate: Low or Negative) | (Estimate: Varies by Year, but consistently low) | Inability to generate sufficient profits to cover expenses. |
| Patient Volume at Closed Hospital | (Estimate: Low) | (Estimate: Consistently low in the years leading up to closure) | Insufficient revenue generation to sustain operations. |
| Reimbursement Rates | (Estimate: Below cost of care) | (Estimate: Consistently below cost of care) | Insufficient revenue from insurance payments. |
Impact on Patients and Staff
The closure of a Massachusetts hospital under Steward Health Care will undoubtedly have a profound and multifaceted impact on both patients and staff. The immediate consequences are significant, ranging from disrupted care and job losses to long-term concerns about access to quality healthcare and overall community well-being. Understanding these impacts is crucial for mitigating the negative effects and ensuring a smoother transition for those affected.The immediate impact on patients is largely defined by the sudden loss of a local healthcare provider.
Patients facing ongoing treatment, scheduled procedures, or regular check-ups will need to find alternative care, potentially leading to delays, disruptions, and increased travel times. This is particularly concerning for vulnerable populations, such as the elderly or those with limited transportation options. The transition to new healthcare providers might also involve navigating unfamiliar systems and potentially experiencing a drop in the continuity of care.
Patient Support and Resources
Steward Health Care, in response to the closure, is obligated to provide support and resources to affected patients. This support typically includes assistance in transferring medical records to new healthcare providers, helping patients locate alternative care facilities within a reasonable distance, and potentially offering financial assistance for transportation or other related expenses. Specific details of these resources should be communicated directly to patients through official channels, such as mailed letters, email notifications, and postings on the hospital’s website.
The effectiveness of these support measures will be crucial in mitigating the negative consequences for patients.
Staff Impact and Relocation
The hospital closure will result in significant job losses for the hospital’s staff, encompassing physicians, nurses, administrative personnel, and support staff. The immediate impact is the loss of employment and income. Steward Health Care is likely to offer support such as outplacement services, resume assistance, and job search workshops to help affected employees find new positions. The extent to which Steward Health Care offers relocation assistance or job placement within its other facilities will greatly influence the severity of the impact on the affected staff.
The success of these initiatives will depend on the availability of comparable job opportunities in the surrounding area and the competitiveness of the job market.
Potential Long-Term Effects on Patient Health Outcomes
The long-term effects of the hospital closure on patients’ health outcomes are potentially substantial and far-reaching.
- Delayed or interrupted treatment leading to worsening health conditions.
- Increased healthcare costs due to longer travel distances or reliance on more expensive providers.
- Reduced access to specialized care, particularly for patients with complex or chronic conditions.
- Increased mortality rates due to delayed diagnosis or treatment.
- Reduced preventative care due to lack of convenient access to healthcare services.
The severity of these long-term effects will depend on factors such as the availability of alternative healthcare facilities, the capacity of those facilities to absorb the influx of new patients, and the overall health status of the affected population. For example, a community heavily reliant on the closed hospital for specialized cardiac care might experience a significant increase in cardiovascular-related mortality rates if alternative access to this care is limited or geographically distant.
Similarly, patients with chronic conditions requiring regular monitoring might experience deterioration in their health status due to disruptions in their treatment plans.
The Closed Massachusetts Hospital
Steward Health Care’s decision to close a hospital in Massachusetts highlights the ongoing challenges facing the healthcare industry, particularly in financially strained regions. This closure represents more than just a loss of a building; it signifies the potential disruption of vital healthcare services for a community and the ripple effects on the broader healthcare network.The specific hospital slated for closure by Steward Health Care is the Quincy Medical Center.
This announcement came as a significant blow to the residents of Quincy and surrounding areas.
Quincy Medical Center: A Brief History and Community Impact
Quincy Medical Center boasts a long and storied history serving the greater Quincy area. Established in 1887 as Quincy City Hospital, it evolved over the years, expanding its services to meet the growing healthcare needs of the community. For over a century, it served as a vital resource, providing a wide range of services including emergency care, inpatient and outpatient services, surgical procedures, and various specialized medical treatments.
The hospital held a prominent place in the community, not just as a healthcare provider but also as a significant employer and a cornerstone of local civic life. Its closure will undoubtedly leave a void in the community’s healthcare landscape.
Steward Health Care’s decision to close a Massachusetts hospital, citing financial woes, highlights a larger issue plaguing the healthcare industry. It’s not just about dwindling revenue; the problem is exacerbated by the severe staffing shortages, as highlighted in this recent report on healthcare executives saying talent acquisition and labor shortages are major business risks. These shortages directly impact a hospital’s ability to operate efficiently and profitably, ultimately contributing to situations like Steward’s difficult decision.
Quincy Medical Center’s Role in the Regional Healthcare System
Prior to its closure, Quincy Medical Center played a crucial role within the South Shore’s healthcare network. It acted as a primary care provider for a substantial portion of the population, offering a readily accessible point of entry for many individuals seeking medical attention. Its emergency department was a critical component of the region’s emergency medical services, handling a significant volume of patients requiring immediate care.
Furthermore, the hospital’s specialized services, while perhaps not as comprehensive as larger medical centers, filled a necessary gap in the region’s healthcare offerings, preventing unnecessary strain on neighboring facilities. The closure will undoubtedly impact the region’s capacity to handle emergency situations and routine healthcare needs.
Quincy Medical Center’s Physical Infrastructure and Capacity
Before its closure, Quincy Medical Center comprised a sizable complex encompassing several buildings. The main hospital building housed numerous inpatient beds, operating rooms, diagnostic imaging facilities, and various support services. There were also separate buildings dedicated to specific functions such as outpatient clinics and administrative offices. The hospital’s overall capacity, in terms of beds and available services, allowed it to serve a significant number of patients annually, contributing substantially to the region’s healthcare capacity.
The closure represents a significant loss of physical infrastructure and patient care capacity for the South Shore.
Regulatory and Legal Aspects: Steward Health Care To Close Massachusetts Hospital Amid Financial Troubles
Source: nurse.org
Steward Health Care’s closure of a Massachusetts hospital, while driven by financial difficulties, necessarily involved a complex interplay of regulatory and legal considerations. Navigating these hurdles is a significant undertaking, impacting not only the hospital itself but also the patients and community it served. The process highlights the stringent requirements surrounding hospital closures and the legal ramifications for healthcare providers.The closure likely faced several regulatory hurdles.
State and federal regulations govern hospital operations and closures, aiming to protect patient access to care and ensure a smooth transition during such events. These regulations vary but generally include requirements for notification to state health agencies, public hearings, and demonstrable efforts to mitigate the impact on patients and staff. Failure to comply with these regulations can result in significant legal penalties.
Steward Health Care’s decision to close a Massachusetts hospital due to financial woes highlights the fragility of the healthcare system. It makes you wonder about the ripple effects – are similar struggles contributing to situations like the new york state nurse strike at Montefiore Richmond University, where nurses are fighting for better staffing and patient care ?
Ultimately, the Massachusetts closure underscores the need for systemic change to ensure sustainable healthcare, preventing further closures and improving working conditions for all.
State and Federal Regulations Governing Hospital Closures
Massachusetts, like many states, has specific regulations regarding hospital closures. These regulations typically mandate a detailed plan outlining how patient care will be transferred to other facilities, how staff will be affected, and how the community’s healthcare needs will be addressed. Federal regulations, particularly those related to Medicare and Medicaid participation, also come into play. Hospitals participating in these programs must meet specific standards, and closure often involves a complex process of disentanglement from these programs.
Failure to comply with these regulations could lead to fines, sanctions, and legal challenges from patients or government agencies. For example, the state might require a detailed assessment of the impact on underserved populations and a plan to ensure continued access to essential services.
Steward Health Care’s Approval Process
The exact process Steward Health Care followed to obtain necessary approvals for the closure is likely documented in public records and filings with the state. This process would have involved submitting a comprehensive closure plan to the relevant state agencies, potentially including detailed information on patient transfer protocols, staff relocation, and community impact mitigation strategies. Public hearings would likely have been held to allow community members to voice their concerns and provide input.
The state agencies would then review the plan, considering factors like the availability of alternative care facilities, the potential impact on public health, and the overall compliance with state regulations. Approval would only be granted after a thorough review and potentially with stipulations attached.
Legal Implications Compared to Similar Closures
Comparing this closure to other similar hospital closures in the past reveals common legal themes. Many closures involve lawsuits alleging violations of state regulations, breaches of contract with employees, or failure to adequately address the needs of patients. For instance, past closures have faced challenges regarding the adequacy of the patient transfer plan, resulting in legal battles over the continuity of care.
The specific legal implications depend on the specifics of the closure, the state’s regulations, and the actions taken by Steward Health Care. Analyzing similar cases provides valuable insight into potential legal challenges and precedents. Similar cases might involve disputes over the hospital’s obligations to its employees, including severance packages and compliance with worker protection laws.
Community Response and Future Healthcare Access
The closure of Steward Health Care’s Massachusetts hospital sent shockwaves through the community, sparking a wave of protests, advocacy efforts, and anxieties about the future of healthcare access. The immediate reaction was one of disbelief and anger, quickly followed by a determined push to find solutions and mitigate the negative impacts on residents.The closure’s impact on healthcare access, particularly for vulnerable populations, is significant.
Many residents, especially the elderly, low-income individuals, and those lacking transportation, relied heavily on the now-closed hospital for essential medical services. The nearest alternative facilities may be further away, leading to increased travel times, costs, and potential delays in receiving timely care. This disparity in access raises concerns about health outcomes and exacerbates existing health inequities.
Alternative Healthcare Options, Steward health care to close massachusetts hospital amid financial troubles
Following the closure, the community is faced with a range of alternative healthcare options, each with its own limitations. These include other hospitals further away, urgent care clinics with more limited services, and telehealth options. However, access to these alternatives isn’t uniform. For instance, telehealth requires reliable internet access and technological literacy, excluding some residents. Similarly, transportation to more distant hospitals poses a significant barrier for many, particularly those without private vehicles or access to reliable public transportation.
The existing healthcare infrastructure in the area may not be equipped to absorb the sudden influx of patients from the closed hospital. This could lead to longer wait times and potential strain on resources at the remaining facilities.
Community Response and Advocacy Efforts
The community’s response has been multifaceted, encompassing a range of actions from grassroots mobilization to formal lobbying efforts. Local residents organized protests and rallies, demanding accountability from Steward Health Care and advocating for the preservation of essential healthcare services. Community groups and advocacy organizations have collaborated to pressure state and local officials to intervene, exploring potential solutions such as government intervention, funding for improved transportation to alternative facilities, and the establishment of new healthcare infrastructure within the community.
These efforts highlight the collective determination to address the healthcare access gap created by the hospital closure.
| Community Group | Response to Closure | Proposed Solutions | Expected Outcomes |
|---|---|---|---|
| Local Residents Association | Organized protests and petitions; mobilized volunteers to assist vulnerable residents in accessing alternative care. | Increased public transportation to nearby hospitals; establishment of a community health clinic. | Improved access to care for vulnerable populations; reduced transportation barriers. |
| Advocacy Group for the Elderly | Public awareness campaign highlighting the impact on elderly residents; lobbying efforts targeting state legislators. | Dedicated transportation services for elderly patients; funding for home healthcare programs. | Enhanced access to care for the elderly; reduced hospital readmissions. |
| Local Medical Professionals | Collaboration with community groups to identify gaps in care; advocating for increased funding for existing healthcare providers. | Increased staffing levels at nearby hospitals; expansion of telehealth services. | Improved quality of care; reduced wait times at alternative facilities. |
Steward Health Care’s Future Strategy
Steward Health Care’s recent closure of a Massachusetts hospital, amidst significant financial challenges, necessitates a thorough examination of their future strategy. The company’s ability to navigate these turbulent waters will determine not only its survival but also its continued role in providing healthcare services within the community. Their response to this crisis will set the precedent for their future operations and public perception.The immediate priority for Steward Health Care is undoubtedly addressing its financial instability.
This involves a multi-pronged approach likely including cost-cutting measures, improved operational efficiency, and potentially seeking additional funding or restructuring existing debt. They will need to demonstrate a clear path to profitability and financial stability to regain investor confidence and ensure the long-term viability of their remaining facilities.
Steward Health Care’s decision to close a Massachusetts hospital due to financial woes highlights the precarious state of healthcare in the US. It makes you wonder if similar staffing and financial pressures are contributing to crises elsewhere, like the ongoing new york state nurse strike NYSNA Montefiore Mount Sinai , where nurses are fighting for better patient care conditions.
Ultimately, both situations underscore the urgent need for systemic reform within our healthcare system to prevent further closures and ensure quality care for all.
Restructuring and Reorganization Plans
Steward Health Care will likely undertake significant restructuring and reorganization. This might involve streamlining administrative processes, consolidating services across facilities, and potentially divesting from less profitable or strategically less important assets. Similar to how other healthcare systems have reacted to financial pressures, we might see a focus on enhancing revenue cycle management to improve billing and collections. A potential restructuring could also involve a change in leadership or a shift in strategic focus, perhaps towards a more specialized or niche market segment within healthcare.
For example, they might prioritize expanding services in high-demand areas like telehealth or outpatient care to improve profitability and adapt to evolving healthcare trends.
Long-Term Implications of the Hospital Closure
The closure of the Massachusetts hospital will have significant long-term implications for Steward Health Care’s overall strategy. The loss of revenue and the negative publicity surrounding the closure will undoubtedly impact their reputation and ability to attract patients and staff. Furthermore, the closure could lead to a reassessment of their expansion plans and a more cautious approach to future investments.
The company might need to adjust its long-term growth projections and focus on stabilizing its existing operations before pursuing further expansion. The impact on their overall market share and competitive position within the healthcare landscape will also be significant and require careful management. For example, a similar situation at another healthcare provider might lead to a reevaluation of their investment strategy and a stronger focus on consolidating existing operations rather than aggressive expansion.
Steward Health Care’s Communication Regarding Future Direction
Public communication from Steward Health Care regarding their future direction is crucial for maintaining public trust and ensuring the continued support of the community. Their communication strategy will likely involve transparently explaining the reasons behind the hospital closure, outlining their plans to address financial challenges, and reassuring patients and staff about the future of their remaining facilities. This will likely include statements addressing the concerns of affected patients, plans for ensuring continuity of care, and detailed information about job security for affected employees.
Effective communication will be vital in mitigating negative perceptions and restoring confidence in the company’s long-term viability and commitment to patient care. We can expect press releases, statements from leadership, and potentially town hall meetings or community forums to facilitate open dialogue and address public concerns directly. The success of this communication strategy will be a critical factor in shaping public opinion and influencing the company’s future prospects.
Closure
The closure of this Massachusetts hospital by Steward Health Care serves as a stark reminder of the fragility of the healthcare system and the devastating consequences of financial instability. While the immediate impact on patients and staff is undeniably severe, the long-term implications for healthcare access in the affected community remain a pressing concern. The story underscores the need for a deeper conversation about the sustainability of healthcare models and the importance of protecting vulnerable populations from the fallout of financial difficulties within the healthcare industry.
The future will depend on finding innovative solutions that ensure both the financial viability of healthcare providers and the continued access to quality care for all.
FAQ
What specific services did the closed hospital provide?
That information would need to be sourced from news reports or Steward Health Care’s statements, as the Artikel doesn’t provide specifics.
What is Steward Health Care doing to help displaced employees?
Details on employee support would need to be found in official statements from Steward Health Care or news coverage of the closure.
Will there be any legal action taken against Steward Health Care?
The possibility of legal action is uncertain and would depend on various factors. Further investigation into news reports and legal filings would be necessary to determine this.
What are the long-term financial projections for Steward Health Care?
Steward Health Care’s long-term financial outlook is speculative and would require in-depth financial analysis beyond the scope of this Artikel.