What is Steroid-Induced Diabetes? Know the Common Side Effect
What is steroid induced diabetes know common side effect – What is steroid-induced diabetes? Knowing this common side effect of steroid use is crucial for anyone taking these powerful medications. Steroids, while incredibly helpful in treating various conditions, can unfortunately disrupt your body’s natural blood sugar regulation, leading to hyperglycemia – high blood sugar. This isn’t quite the same as type 1 or type 2 diabetes, though it shares some similar symptoms and risks.
Let’s delve into understanding how steroids impact your body and what you can do to mitigate the risks.
This post will cover the mechanisms behind steroid-induced diabetes, the groups most at risk, how it’s diagnosed, effective management strategies (including lifestyle changes and medication), potential long-term complications, and crucially, preventative measures. We’ll even look at real-life case studies to illustrate the importance of proactive management. Get ready to become a well-informed advocate for your own health!
Definition and Mechanisms of Steroid-Induced Diabetes
Steroid-induced diabetes, also known as steroid diabetes, is a form of hyperglycemia that develops as a side effect of corticosteroid use. It’s a temporary condition that usually resolves once steroid treatment is stopped, unlike type 1 and type 2 diabetes, which are chronic conditions. Understanding the mechanisms behind steroid-induced diabetes is crucial for effective management and preventing long-term complications.Steroid-induced hyperglycemia arises primarily due to the impact of glucocorticoids on glucose metabolism.
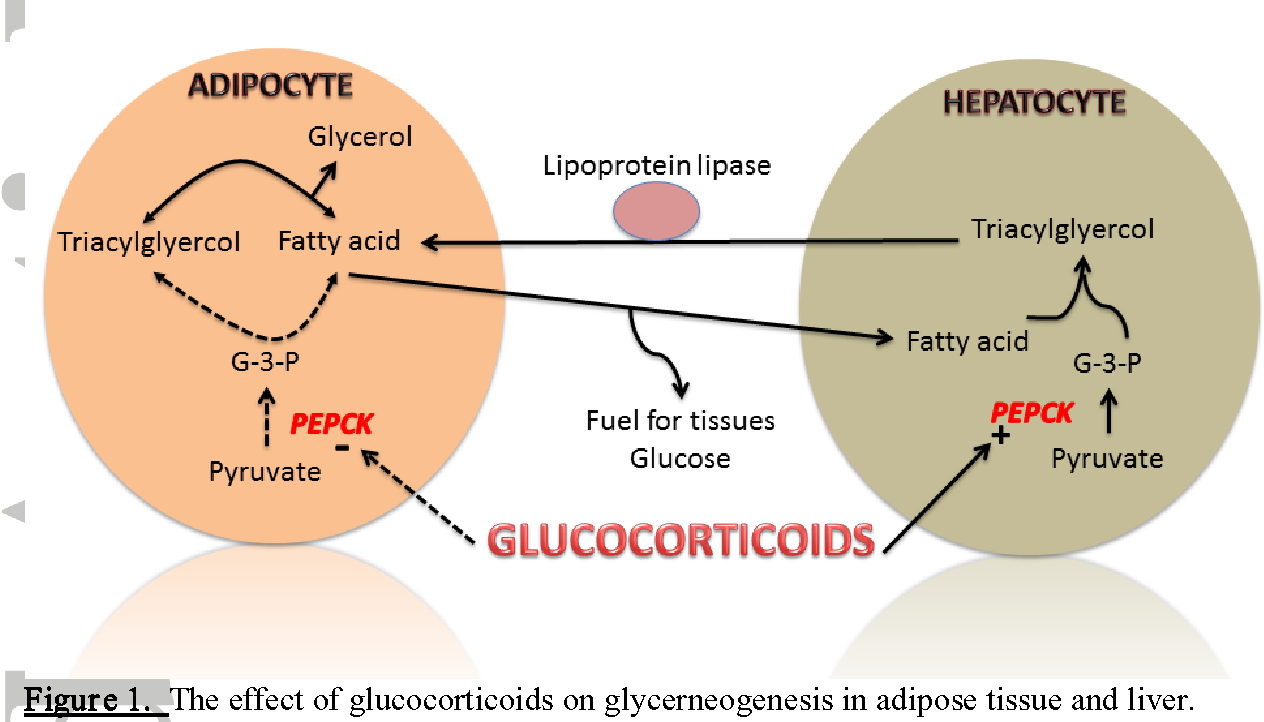
Glucocorticoids, such as cortisol, exert multiple effects that disrupt the body’s normal glucose regulation. They increase hepatic glucose production (gluconeogenesis) by stimulating the liver to produce more glucose from non-carbohydrate sources like amino acids and glycerol. Simultaneously, they decrease glucose uptake by peripheral tissues (like muscle and fat cells), leading to elevated blood glucose levels. This happens because glucocorticoids reduce the sensitivity of these tissues to insulin, a hormone responsible for facilitating glucose uptake.
Furthermore, glucocorticoids can also increase insulin resistance, meaning that even when insulin is present, it’s less effective at lowering blood sugar.
Mechanisms of Steroid-Induced Diabetes Compared to Type 1 and Type 2 Diabetes
Steroid-induced diabetes differs significantly from type 1 and type 2 diabetes in its underlying mechanisms. Type 1 diabetes is an autoimmune disease where the body’s immune system attacks and destroys insulin-producing cells in the pancreas, leading to absolute insulin deficiency. Type 2 diabetes, on the other hand, is characterized by insulin resistance, where the body’s cells don’t respond effectively to insulin, often combined with a relative deficiency in insulin production.
So, steroid-induced diabetes is a nasty side effect of some medications, seriously impacting blood sugar levels. Managing this often involves dietary changes, and that’s where understanding nutritional needs becomes crucial. It’s fascinating to learn more about how different sexes metabolize food, like in this article on are women and men receptive of different types of food and game changing superfoods for women , which highlights the importance of personalized nutrition plans.
This knowledge is especially relevant when dealing with the dietary restrictions often necessary for managing steroid-induced diabetes.
Steroid-induced diabetes, however, is a state of insulin resistance primarily caused by the direct actions of glucocorticoids on glucose metabolism, without the autoimmune component of type 1 or the progressive beta-cell dysfunction of type 2. It’s essentially a pharmacologically induced state of relative insulin resistance and increased glucose production.
Metabolic Pathways Affected by Steroid Use
Steroid use significantly alters several key metabolic pathways. As mentioned, gluconeogenesis is dramatically increased, leading to excessive glucose production by the liver. Glycogenolysis, the breakdown of glycogen (stored glucose) in the liver and muscles, is also stimulated, further contributing to elevated blood glucose levels. Simultaneously, peripheral glucose uptake is reduced due to impaired insulin signaling, resulting in glucose remaining in the bloodstream.
Lipogenesis (fat synthesis) is also affected, with increased fat deposition in certain areas of the body. This complex interplay of metabolic changes results in the characteristic hyperglycemia of steroid-induced diabetes.
Hormonal Changes in Steroid-Induced Diabetes
The following table summarizes the key hormonal changes observed in steroid-induced diabetes:
| Hormone | Effect of Steroid Use | Impact on Glucose Metabolism | Comparison to Type 1 & 2 Diabetes |
|---|---|---|---|
| Cortisol | Increased levels | Increased gluconeogenesis, decreased glucose uptake, increased insulin resistance | Elevated in some cases of type 2, but not the primary cause |
| Insulin | Increased secretion (initially), but ultimately ineffective due to resistance | Decreased effectiveness in lowering blood glucose | Deficient in type 1, relatively deficient or resistant in type 2 |
| Glucagon | Potentially increased | Further stimulates gluconeogenesis and glycogenolysis | Can be elevated in both type 1 and type 2 |
| Growth Hormone | Potentially increased | Contributes to insulin resistance and increased gluconeogenesis | Can be altered in both type 1 and type 2, but not the primary driver |
Prevalence and Risk Factors
Steroid-induced diabetes (SID) is a significant concern for individuals requiring glucocorticoid therapy. Understanding its prevalence and the factors that increase susceptibility is crucial for effective management and prevention. This section will explore the populations most at risk, the influence of dosage and duration of steroid use, and the interplay between steroid use and pre-existing conditions.The prevalence of SID varies considerably depending on several factors, making it difficult to pinpoint a single, universally applicable figure.
However, studies consistently demonstrate a clear link between glucocorticoid use and the development of hyperglycemia. This relationship is particularly pronounced with higher doses and longer durations of treatment.
Groups Most Susceptible to Developing Steroid-Induced Diabetes
Several groups are more vulnerable to developing SID than others. These include individuals with a family history of diabetes, those with a pre-existing condition that increases diabetes risk (such as obesity or polycystic ovary syndrome), and older adults. Ethnic background may also play a role, with some populations showing higher susceptibility. The underlying mechanisms driving this increased vulnerability are complex and not fully understood, but likely involve a combination of genetic predisposition and the amplified effects of glucocorticoids on glucose metabolism.
Dosage and Duration of Steroid Use and Increased Risk
The risk of developing SID is directly correlated with both the dosage and duration of glucocorticoid therapy. Higher doses of steroids lead to a more significant disruption of glucose homeostasis. Similarly, prolonged use increases the cumulative effect on the body’s ability to regulate blood sugar. For instance, a patient receiving a high dose of prednisone for several months has a considerably higher risk of developing SID compared to someone receiving a low dose for a short period.
This highlights the importance of careful monitoring of blood glucose levels in individuals undergoing steroid treatment.
Interaction Between Steroid Use and Pre-existing Conditions
Pre-existing conditions significantly influence the likelihood of developing SID. Obesity, for example, is a well-established risk factor for both type 2 diabetes and SID. The combination of steroid use and obesity creates a synergistic effect, substantially increasing the risk of hyperglycemia. Similarly, conditions like polycystic ovary syndrome (PCOS) and acromegaly are associated with insulin resistance, making individuals with these conditions particularly vulnerable to SID.
Existing insulin resistance from these pre-existing conditions means that the body is less efficient at using insulin, exacerbating the effects of glucocorticoids on glucose metabolism. Therefore, careful management of pre-existing conditions is crucial in mitigating the risk of SID in patients requiring steroid therapy.
Symptoms and Diagnosis: What Is Steroid Induced Diabetes Know Common Side Effect
Source: mdpi-res.com
Steroid-induced diabetes, while sharing similarities with other forms of diabetes, presents a unique set of challenges in terms of diagnosis and management. Understanding the typical symptoms and diagnostic procedures is crucial for timely intervention and effective control of blood glucose levels. This section will Artikel the common symptoms, diagnostic tests, and a step-by-step approach to diagnosis.
Recognizing the symptoms of steroid-induced diabetes is the first step towards effective management. Early detection can prevent or minimize the long-term complications associated with uncontrolled blood sugar. The symptoms can be subtle and may mimic those of other conditions, making accurate diagnosis critical.
Steroid-induced diabetes is a nasty side effect, often cropping up in folks needing immunosuppressants after organ transplants. It makes you wonder about the long-term health implications, especially considering the huge news that the FDA approved clinical trials for pig kidney transplants in humans, as reported here: fda approves clinical trials for pig kidney transplants in humans. This development raises questions about the necessary immunosuppression levels and the potential increase in steroid-induced diabetes cases down the line.
Common Symptoms of Steroid-Induced Diabetes
The symptoms of steroid-induced diabetes are often similar to those of type 2 diabetes, but can sometimes be less pronounced or even absent in the early stages. It’s important to note that the severity of symptoms can vary greatly from person to person.
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Increased hunger (polyphagia)
- Unexplained weight loss
- Fatigue and weakness
- Blurred vision
- Slow-healing sores
- Increased susceptibility to infections
Diagnostic Tests for Steroid-Induced Diabetes
Several tests are used to confirm a diagnosis of steroid-induced diabetes. These tests help determine the extent of glucose intolerance and guide treatment strategies.
- Fasting Plasma Glucose (FPG): Measures blood glucose levels after an overnight fast. A FPG level of ≥126 mg/dL on two separate occasions indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): Measures blood glucose levels at intervals after consuming a sugary drink. A 2-hour post-load glucose level of ≥200 mg/dL indicates diabetes.
- HbA1c (Glycated Hemoglobin): Measures the average blood glucose levels over the past 2-3 months. An HbA1c level of ≥6.5% indicates diabetes.
- Random Plasma Glucose (RPG): Measures blood glucose at any time of day, regardless of when the last meal was eaten. A RPG level of ≥200 mg/dL along with classic symptoms strongly suggests diabetes.
Comparison of Symptoms with Other Forms of Diabetes
While the symptoms of steroid-induced diabetes overlap significantly with those of type 1 and type 2 diabetes, some subtle differences exist. Steroid-induced diabetes often develops more rapidly than type 2 diabetes and may not always present with the classic symptoms of excessive thirst and urination. In contrast to type 1 diabetes, steroid-induced diabetes is not typically associated with autoimmune destruction of pancreatic beta cells.
Step-by-Step Diagnostic Process
Diagnosing steroid-induced diabetes involves a systematic approach that combines clinical evaluation and laboratory testing. The process is designed to rule out other causes of hyperglycemia and to determine the severity of the condition.
- Medical History and Physical Examination: The physician will review the patient’s medical history, focusing on steroid use, family history of diabetes, and the presence of any symptoms.
- Initial Blood Glucose Test: A fasting plasma glucose (FPG) test is typically performed to assess baseline blood glucose levels.
- Further Testing (if indicated): If the FPG is elevated or if symptoms are present, further testing, such as an OGTT or HbA1c, may be necessary to confirm the diagnosis and assess the severity of glucose intolerance.
- Diagnosis Confirmation: A diagnosis of steroid-induced diabetes is made based on the results of these tests and the patient’s clinical presentation, taking into account the use of corticosteroids.
Management and Treatment Strategies
Source: cloudfront.net
Managing steroid-induced diabetes (SID) requires a multi-pronged approach focusing on blood glucose control, minimizing long-term complications, and addressing the underlying steroid use. The goal is to maintain blood glucose levels within a healthy range while balancing the need for continued steroid therapy, if necessary. This often involves a combination of lifestyle modifications and medication.
So, steroid-induced diabetes is a nasty side effect – your body’s response to steroids throws your blood sugar levels out of whack. This can lead to serious complications, and it’s crucial to monitor your levels carefully. One of the scary things to consider is that high blood sugar is actually one of the risk factors that make stroke more dangerous , making managing steroid-induced diabetes even more vital for overall health.
Therefore, keeping those blood sugar levels in check is paramount to preventing further health issues.
Lifestyle Modifications, What is steroid induced diabetes know common side effect
Lifestyle changes are crucial in managing SID. These adjustments help improve insulin sensitivity and overall metabolic health. A significant part of this involves careful dietary management and regular physical activity. The effectiveness of these changes is directly linked to the individual’s adherence and the severity of their SID. For example, a patient with mild SID might achieve good control with dietary changes alone, whereas a patient with more severe hyperglycemia may require medication in addition to lifestyle changes.
Dietary Management
A well-planned diet is fundamental. This usually entails a balanced approach focused on consuming complex carbohydrates, lean proteins, and healthy fats. Portion control is essential to avoid spikes in blood glucose levels. Individuals with SID should focus on consuming foods with a low glycemic index (GI), which means they cause a slower, more gradual rise in blood sugar.
This might involve substituting refined grains with whole grains, choosing fruits lower in sugar, and limiting sugary drinks and processed foods. A registered dietitian can provide personalized guidance on creating a suitable meal plan tailored to the individual’s needs and preferences.
Exercise Recommendations
Regular physical activity plays a vital role in improving insulin sensitivity and managing blood glucose levels. At least 150 minutes of moderate-intensity aerobic exercise per week is generally recommended. This could include brisk walking, swimming, cycling, or other activities the individual enjoys. Incorporating strength training exercises two or three times a week is also beneficial for overall health and metabolic function.
The type and intensity of exercise should be tailored to the individual’s fitness level and any underlying health conditions. It’s important to consult a healthcare professional before starting any new exercise program.
Medication Management
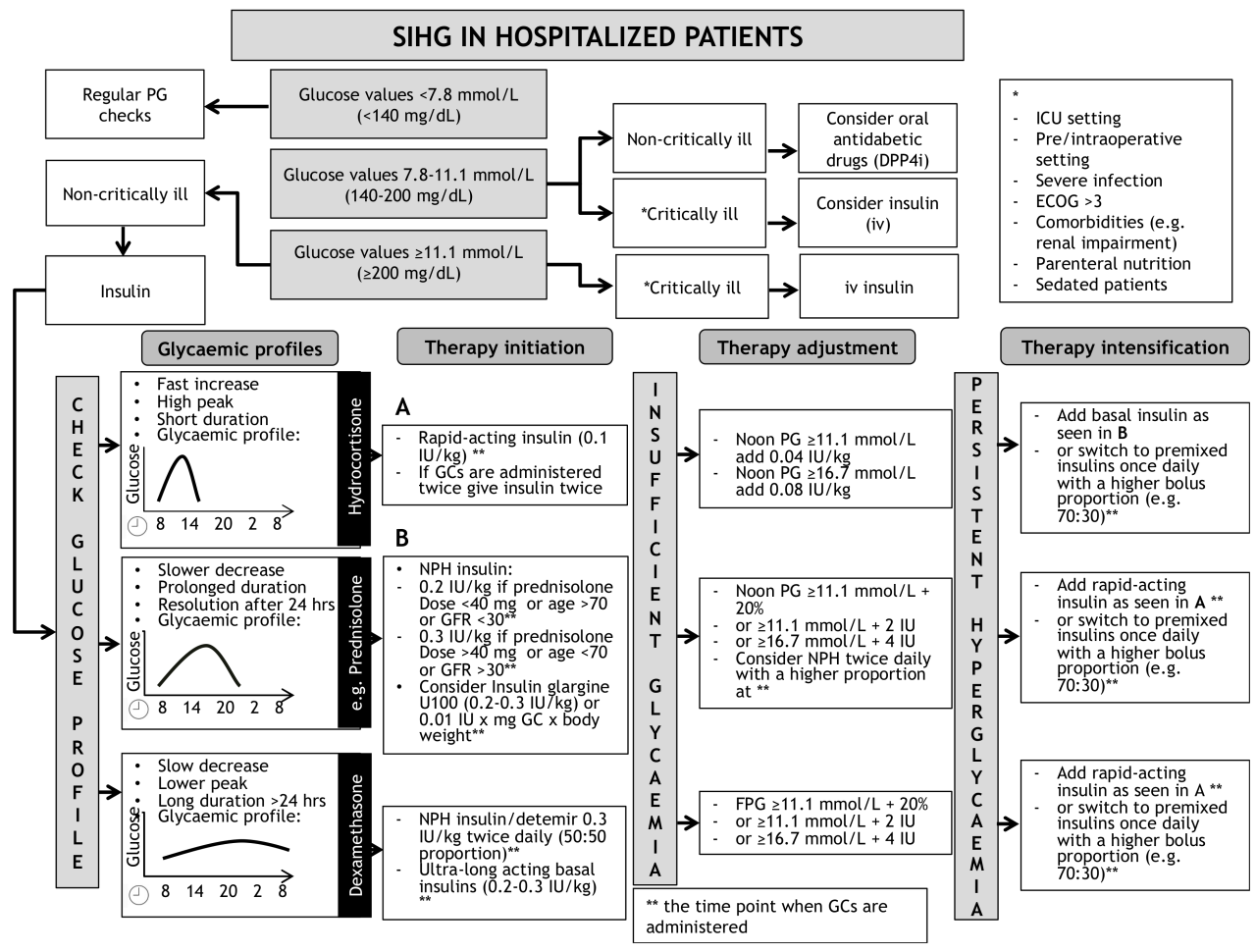
When lifestyle modifications alone are insufficient to control blood glucose levels, medication becomes necessary. The choice of medication depends on several factors, including the severity of hyperglycemia, the individual’s overall health, and the duration of steroid use.
Insulin Therapy
Insulin may be required if blood glucose levels remain high despite lifestyle modifications. The type and dosage of insulin will be determined by a healthcare professional based on the individual’s needs. Insulin injections or insulin pumps can effectively regulate blood glucose levels. Close monitoring of blood glucose levels is crucial to ensure optimal insulin dosing.
Oral Hypoglycemic Agents
In some cases, oral hypoglycemic agents might be considered as an alternative or in addition to lifestyle modifications. Metformin is often the first-line oral medication for type 2 diabetes and is sometimes used in SID, though its efficacy can be limited. Other oral agents might be used depending on the individual’s response and other health factors. However, the use of oral hypoglycemics in SID is often less effective than insulin therapy, and insulin is generally preferred for better blood glucose control.
Sample Treatment Plan
A sample treatment plan for a 45-year-old male with SID induced by high-dose prednisone for autoimmune disease, showing moderately elevated blood glucose levels, might include:* Dietary Changes: A low-glycemic index diet emphasizing whole grains, lean proteins, and healthy fats, with portion control and limited intake of sugary drinks and processed foods. Consultation with a registered dietitian to personalize this plan.
Exercise
30 minutes of brisk walking most days of the week, along with twice-weekly strength training sessions.
Medication
Initially, metformin might be tried. If blood glucose control remains inadequate after several weeks, insulin therapy would likely be initiated, starting with a basal insulin regimen and potentially adding bolus insulin as needed.
Monitoring
Regular blood glucose monitoring (several times daily) to adjust medication dosage as needed and assess the effectiveness of the treatment plan. Regular follow-up appointments with an endocrinologist or diabetes specialist to review progress and make adjustments to the treatment plan.
Long-Term Complications
Steroid-induced diabetes, while often resolving upon cessation of steroid use, can unfortunately leave behind a legacy of long-term health problems. The duration and intensity of steroid exposure, along with pre-existing risk factors, significantly influence the likelihood and severity of these complications. Understanding these potential consequences is crucial for effective management and prevention.The risks associated with long-term complications in steroid-induced diabetes are comparable to, and in some cases may even exceed, those seen in type 2 diabetes.
This is because the high blood glucose levels induced by steroids can damage various organs over time, leading to a range of serious health issues. The rapid onset and sometimes significant hyperglycemia contribute to this increased risk profile. Moreover, individuals already predisposed to cardiovascular disease are particularly vulnerable to accelerated damage.
Cardiovascular Health Impact
Steroid-induced diabetes significantly elevates the risk of cardiovascular disease (CVD). High blood sugar levels damage blood vessels, leading to atherosclerosis (hardening of the arteries), increasing the chances of heart attack, stroke, and peripheral artery disease. Furthermore, steroids themselves can have direct negative effects on the cardiovascular system, impacting blood pressure and lipid profiles. For example, a patient with pre-existing hypertension who is prescribed a course of corticosteroids might experience a significant and rapid worsening of their blood pressure, placing them at much greater risk of stroke or heart failure.
The combined effect of hyperglycemia and the direct cardiovascular effects of steroids creates a potent risk factor for serious cardiovascular events. Managing blood sugar and blood pressure meticulously is paramount to mitigating this risk.
Long-Term Complications Summary
The following table summarizes the potential long-term complications of steroid-induced diabetes and their management strategies. Effective management requires a multi-faceted approach involving lifestyle modifications, medication, and close monitoring.
| Complication | Description | Management | Notes |
|---|---|---|---|
| Cardiovascular Disease (CVD) | Heart disease, stroke, peripheral artery disease due to damaged blood vessels. | Blood pressure control, cholesterol management, lifestyle changes (diet, exercise), antiplatelet therapy. | Risk is significantly increased compared to non-diabetic populations. |
| Nephropathy (Kidney Disease) | Damage to the kidneys leading to impaired kidney function. | Blood pressure control, blood glucose control, ACE inhibitors or ARBs. | Regular kidney function tests are crucial. |
| Neuropathy (Nerve Damage) | Damage to nerves causing pain, numbness, tingling, and weakness. | Blood glucose control, pain management, lifestyle modifications. | Careful foot care is essential to prevent ulcers. |
| Retinopathy (Eye Damage) | Damage to the blood vessels in the retina, leading to vision loss. | Blood glucose control, regular eye exams, laser treatment if needed. | Early detection and management are crucial to prevent blindness. |
Prevention and Minimizing Risk
Steroid-induced diabetes (SID) is a serious complication, but proactive measures can significantly reduce your risk. Understanding the factors that contribute to SID and adopting preventative strategies is crucial for maintaining good health while undergoing steroid treatment. This section Artikels practical steps you can take to minimize your chances of developing SID and manage your blood glucose effectively.Minimizing the risk of developing SID involves a multifaceted approach focusing on lifestyle modifications, close monitoring, and proactive medical management.
The goal is to mitigate the impact of steroids on your body’s glucose metabolism. This includes both preventative measures before steroid use begins and careful management during treatment.
Lifestyle Modifications to Reduce SID Risk
Adopting a healthy lifestyle before and during steroid treatment is vital in preventing or minimizing the development of SID. This involves making conscious choices about diet, exercise, and overall well-being. These changes can significantly impact your body’s response to steroids.
- Dietary Adjustments: A balanced diet low in refined carbohydrates and saturated fats is essential. Focus on whole grains, lean proteins, fruits, and vegetables. This helps regulate blood sugar levels and improves insulin sensitivity. For example, swapping sugary drinks for water or unsweetened tea can make a substantial difference.
- Regular Physical Activity: Regular exercise improves insulin sensitivity and helps control blood sugar levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Activities like brisk walking, swimming, or cycling are beneficial.
- Weight Management: Maintaining a healthy weight reduces the risk of developing insulin resistance, a key factor in SID. If you are overweight or obese, losing even a small amount of weight can significantly improve your glucose control.
Regular Blood Glucose Monitoring During Steroid Therapy
Regular monitoring of blood glucose levels is paramount during steroid treatment. This allows for early detection of any abnormalities and timely intervention to prevent the development of SID or manage existing hyperglycemia.Frequent blood glucose testing provides a clear picture of how your body is responding to the steroids. This allows for adjustments to medication or lifestyle as needed. The frequency of testing will depend on your individual risk factors and your doctor’s recommendations.
For example, some individuals might require daily testing, while others may only need testing a few times a week.
Patient Education: A Cornerstone of SID Prevention
Patient education plays a crucial role in preventing and managing SID. Understanding the risks, recognizing the symptoms, and knowing how to manage your blood sugar are essential for effective self-care. Empowering patients with knowledge and tools helps them actively participate in their healthcare.A well-informed patient is better equipped to make healthy lifestyle choices, adhere to treatment plans, and effectively communicate with their healthcare provider.
This collaborative approach significantly improves the chances of successful management and reduces the long-term complications associated with SID.
Patient Education Plan: Preventative Measures and Monitoring Techniques
A comprehensive patient education plan should include the following elements:
- Understanding Steroid-Induced Diabetes: A clear explanation of SID, its causes, and potential complications.
- Risk Factor Assessment: Identifying individual risk factors for SID, such as family history of diabetes, obesity, and existing metabolic conditions.
- Lifestyle Modifications: Detailed guidance on dietary changes, exercise recommendations, and weight management strategies.
- Blood Glucose Monitoring: Instruction on how to perform self-monitoring of blood glucose, including the frequency and timing of testing.
- Medication Management: Information on prescribed medications, their purpose, potential side effects, and proper administration.
- Symptom Recognition: Education on recognizing the symptoms of high blood sugar, such as increased thirst, frequent urination, and fatigue.
- Emergency Procedures: Instructions on what to do in case of severe hyperglycemia or other complications.
- Regular Follow-up Appointments: Emphasizing the importance of regular check-ups with their healthcare provider to monitor blood glucose levels and make necessary adjustments to treatment.
Illustrative Case Studies
Source: diabetesonthenet.com
Understanding the nuances of steroid-induced diabetes (SID) requires examining real-world scenarios. The following case studies illustrate both successful management and the potential for complications, highlighting key aspects of prevention and treatment.
Case Study 1: Successful Management of Steroid-Induced Diabetes
This case involves a 55-year-old woman, Mrs. Jones, diagnosed with severe rheumatoid arthritis. She was prescribed a high dose of prednisone (60mg daily) for a severe flare-up. Prior to steroid treatment, Mrs. Jones had no history of diabetes.
After two weeks of prednisone therapy, routine blood tests revealed hyperglycemia (elevated blood sugar) and elevated HbA1c levels, confirming the diagnosis of SID. Her physician immediately initiated a comprehensive management plan. This included close monitoring of blood glucose levels, dietary adjustments emphasizing a low glycemic index diet, and the introduction of metformin, an oral antidiabetic medication. Regular exercise was also encouraged.
Importantly, the prednisone dosage was gradually tapered down over several months under close medical supervision. Mrs. Jones diligently followed her treatment plan. Her blood glucose levels normalized within three months of diagnosis, and her HbA1c levels returned to the normal range. She remained diabetes-free after the prednisone was discontinued.
Case Study 2: Development of Complications from Steroid-Induced Diabetes
Mr. Smith, a 68-year-old man with a history of hypertension and chronic obstructive pulmonary disease (COPD), required a high dose of corticosteroids (methylprednisolone) for an acute exacerbation of his COPD. He had no prior history of diabetes. While on steroids, he experienced significant weight gain, polyuria (increased urination), and polydipsia (increased thirst), classic symptoms of hyperglycemia. Despite these symptoms, Mr.
Smith initially delayed seeking medical attention. When he finally did, his blood glucose levels were dangerously high, and he was diagnosed with SID. Unfortunately, due to the delayed diagnosis and lack of adherence to the prescribed treatment plan (which included insulin therapy and dietary modifications), Mr. Smith developed several complications, including diabetic ketoacidosis (DKA), a life-threatening condition. He required hospitalization for intensive management of his DKA.
Following his recovery, he continued to struggle with blood sugar control and developed peripheral neuropathy (nerve damage). This case highlights the importance of early diagnosis, prompt treatment, and consistent adherence to the prescribed management plan to prevent serious complications associated with SID.
Insights from Case Studies
The contrasting outcomes of these two cases underscore the critical role of proactive monitoring, timely intervention, and patient adherence in managing SID. Mrs. Jones’ successful outcome demonstrates the effectiveness of early diagnosis, a tailored treatment plan that included lifestyle modifications and medication, and consistent follow-up care. In contrast, Mr. Smith’s experience emphasizes the severe consequences of delayed diagnosis and inadequate management, leading to potentially life-threatening complications.
These cases highlight the importance of educating patients about the risks of SID, promoting early detection through regular monitoring, and ensuring patients understand and adhere to their prescribed treatment plans. The importance of a multidisciplinary approach involving endocrinologists, pulmonologists (in cases like Mr. Smith’s), and other specialists, as needed, cannot be overstated.
Ending Remarks
So, while steroid-induced diabetes can be a serious side effect, it’s definitely manageable with the right knowledge and proactive approach. Remember, regular blood glucose monitoring, a healthy lifestyle, and close collaboration with your doctor are key to preventing complications and maintaining overall well-being. Don’t hesitate to ask questions – your health is paramount! Understanding the nuances of steroid-induced diabetes empowers you to take control and live a healthier life, even while managing a condition that requires medication.
Quick FAQs
Can steroid-induced diabetes be reversed?
Often, blood sugar levels return to normal once steroid treatment is stopped. However, in some cases, the condition can persist. Close monitoring and management are essential.
Are all steroids equally likely to cause diabetes?
No, the risk varies depending on the type and dose of steroid used, as well as the duration of treatment. Higher doses and longer treatment periods generally increase the risk.
What if I have a family history of diabetes and need steroids?
If you have a family history of diabetes, you’re at a higher risk of developing steroid-induced diabetes. Your doctor will likely monitor your blood sugar more closely.
Can I exercise if I have steroid-induced diabetes?
Yes, regular exercise is highly beneficial in managing blood sugar levels. However, it’s important to discuss an appropriate exercise plan with your doctor.
