Securing IoT Solutions for Telemedicine
Securing iomt solutions for telemedicine – Securing IoT solutions for telemedicine isn’t just about protecting data; it’s about safeguarding lives. In today’s increasingly connected healthcare landscape, telemedicine relies heavily on the seamless flow of sensitive patient information through various IoT devices. But this connectivity brings inherent risks. From vulnerable wearables to potentially compromised network infrastructure, the potential for breaches and data leaks is significant.
This post dives deep into the critical strategies and technologies needed to secure these vital systems, ensuring patient privacy and the integrity of telehealth services.
We’ll explore the multifaceted nature of securing telemedicine, covering everything from robust encryption methods and secure data storage solutions to the implementation of firewalls, VPNs, and secure access technologies. We’ll also delve into regulatory compliance, user authentication, and incident response planning – all crucial components in building a truly secure telemedicine ecosystem. Get ready to navigate the complexities of securing this rapidly evolving field.
Data Security in Telemedicine IoT Solutions
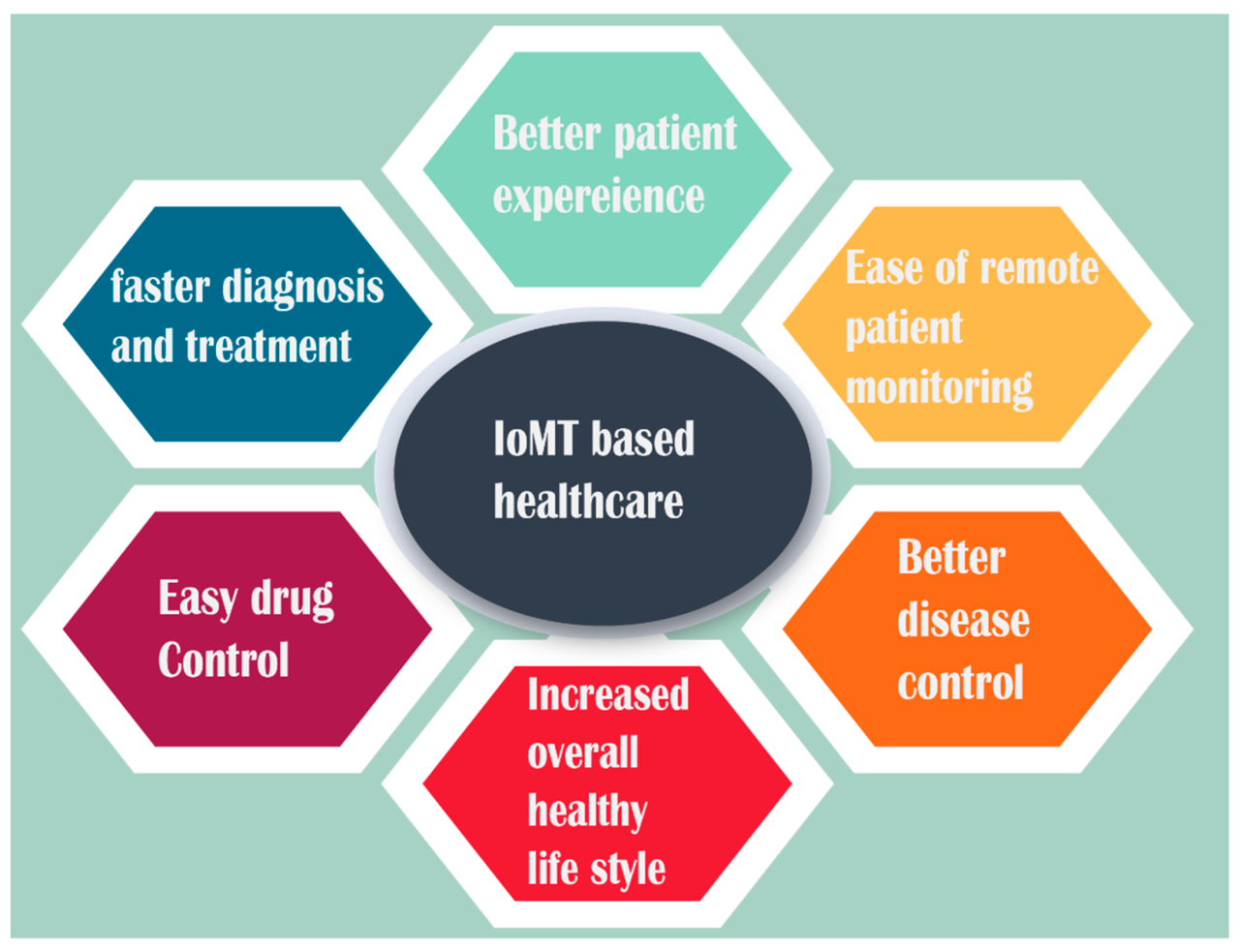
The increasing reliance on Internet of Medical Things (IoMT) devices in telemedicine presents significant opportunities for improved patient care, but also introduces considerable security risks. Protecting sensitive patient data transmitted and stored by these devices is paramount, requiring a multi-layered approach encompassing device security, data encryption, and robust data storage solutions. Failure to adequately address these security concerns can lead to data breaches, identity theft, and compromised patient care.
Vulnerabilities of IoMT Devices and Mitigation Strategies
IoMT devices, ranging from wearable sensors to connected medical equipment, often lack robust security features. Common vulnerabilities include weak default passwords, insufficient authentication mechanisms, unsecured communication channels, and outdated software. These weaknesses make them susceptible to hacking, malware infection, and data manipulation. Mitigation strategies include implementing strong authentication protocols (like multi-factor authentication), regularly updating device firmware and software, employing secure communication protocols (such as TLS/SSL), and utilizing network segmentation to isolate medical devices from other systems.
Regular security audits and penetration testing can also identify and address potential vulnerabilities before they are exploited. Furthermore, choosing devices from reputable manufacturers with a proven track record of security best practices is crucial.
Comparison of Encryption Methods for Patient Data Transmission
Several encryption methods are suitable for securing patient data transmitted via IoMT devices. Symmetric encryption, such as Advanced Encryption Standard (AES), uses a single key for both encryption and decryption, offering fast performance. However, secure key exchange is a critical challenge. Asymmetric encryption, like RSA, uses a pair of keys (public and private), offering better key management but slower processing speeds.
Hybrid approaches, combining symmetric and asymmetric encryption, are often preferred for optimal security and performance. For example, a session key generated using symmetric encryption can be exchanged securely using asymmetric encryption. The choice of encryption method depends on factors such as the sensitivity of the data, the processing power of the devices, and the network bandwidth. For telemedicine applications involving highly sensitive patient data, AES-256 with a robust key management system is generally recommended.
Secure Data Storage Solution for Patient Health Information
A secure data storage solution for patient health information gathered by IoMT devices must adhere to stringent regulatory requirements (like HIPAA in the US and GDPR in Europe) and provide robust security measures. This includes data encryption both in transit and at rest, access control mechanisms based on the principle of least privilege, and regular data backups. A cloud-based solution offers scalability and accessibility but requires careful consideration of data sovereignty and vendor security practices.
On-premise solutions offer greater control over data but require significant investment in infrastructure and security expertise. A hybrid approach, combining cloud and on-premise storage, can provide a balance between security, scalability, and cost-effectiveness. Regular data backups to a geographically separate location are crucial for disaster recovery and business continuity.
| Solution Name | Key Features | Security Measures | Benefits |
|---|---|---|---|
| Cloud-based Storage (e.g., AWS S3, Azure Blob Storage) | Scalability, accessibility, data redundancy | Encryption at rest and in transit, access control lists (ACLs), multi-factor authentication | Cost-effective, easy to manage, high availability |
| On-premise Storage (e.g., SAN, NAS) | High control over data, compliance with strict security policies | Hardware-based encryption, robust firewalls, intrusion detection systems | Enhanced security, data sovereignty |
| Hybrid Cloud Storage | Combines the benefits of cloud and on-premise storage | Data encryption, access control, regular backups, geographically distributed storage | Balance between cost, security, and scalability |
Network Security for Telemedicine IoT Deployments
Source: mdpi-res.com
Securing the network infrastructure in telemedicine is paramount, especially with the proliferation of Internet of Things (IoT) devices. These devices, ranging from wearable sensors to remote patient monitoring equipment, introduce significant security challenges due to their often limited processing power, diverse operating systems, and potential vulnerabilities. Robust network security measures are essential to protect patient data and maintain the integrity of the telemedicine system.The inherent challenges of securing wireless communication networks used in telemedicine, particularly concerning IoT device connectivity, are multifaceted.
The sheer number of connected devices increases the attack surface, while the decentralized nature of these networks makes centralized management and monitoring difficult. Many IoT devices lack robust security features, and their software often isn’t regularly updated, leaving them vulnerable to exploits. Furthermore, the reliance on wireless communication protocols, such as Wi-Fi and Bluetooth, introduces vulnerabilities to eavesdropping and man-in-the-middle attacks.
Finally, the heterogeneity of devices and their operating systems makes implementing uniform security policies a considerable undertaking.
Firewall and Intrusion Detection/Prevention System Implementation
Implementing firewalls and intrusion detection/prevention systems (IDPS) is crucial for establishing a layered security approach. Firewalls act as the first line of defense, filtering network traffic based on pre-defined rules. They control access to the telemedicine network, blocking unauthorized connections and malicious traffic. Intrusion detection systems (IDS) passively monitor network traffic for suspicious activity, generating alerts when potential threats are detected.
Intrusion prevention systems (IPS) take this a step further, actively blocking or mitigating identified threats. For optimal protection, a combination of firewalls and IDPS is recommended, with firewalls controlling access and IDPS monitoring for sophisticated threats that might bypass the firewall’s rules. For example, a firewall could block access from known malicious IP addresses, while an IPS could detect and block attempts to exploit known vulnerabilities in IoT devices.
Regular updates to firewall rules and IDPS signatures are vital to maintain effectiveness against evolving threats.
Secure Access Technologies for Remote Access
Virtual Private Networks (VPNs) play a critical role in securing remote access to patient data via IoT devices. VPNs create an encrypted tunnel between the IoT device and the telemedicine server, protecting data in transit from eavesdropping and interception. This is particularly crucial when accessing sensitive patient information remotely, such as through mobile applications or remote monitoring systems.
Securing IoMT solutions for telemedicine is crucial for patient safety and data privacy, especially considering the increasing reliance on remote healthcare. The recent new york state nurse strike NYSNA Montefiore Mount Sinai highlights the need for robust systems; imagine the impact on patient care if those systems were compromised during a staffing crisis. Therefore, investing in strong security measures for IoMT in telemedicine is not just good practice, it’s essential for maintaining continuity of care.
Multi-factor authentication (MFA) should be implemented alongside VPNs to add an extra layer of security, requiring users to provide multiple forms of authentication before gaining access. For example, a combination of a password and a one-time code generated by an authentication app. Furthermore, the use of strong encryption protocols, such as TLS 1.3 or higher, is vital to ensure the confidentiality and integrity of data transmitted over the VPN.
Securing IoMT solutions for telemedicine is crucial, especially with the increasing reliance on connected devices. A key aspect of this security involves understanding the potential vulnerabilities, and a recent study, study widespread digital twins healthcare , highlights the need for robust data protection strategies within these systems. Ultimately, strengthening security protocols is paramount to ensuring patient privacy and the overall success of telemedicine initiatives.
Access control lists (ACLs) should be carefully configured to limit access to only authorized users and devices, minimizing the risk of unauthorized access. Regular security audits and penetration testing are recommended to identify and address potential vulnerabilities in the VPN infrastructure and associated access control mechanisms. A real-world example would be a cardiologist remotely monitoring a patient’s heart rate via a wearable sensor; the VPN ensures the data transmission is secure and confidential.
Device Security and Management in Telemedicine
The increasing reliance on Internet of Medical Things (IoMT) devices in telemedicine presents significant security challenges. These devices, ranging from simple wearables to complex remote patient monitoring systems, collect and transmit sensitive patient data, making them prime targets for cyberattacks. Effective security measures are crucial to protect patient privacy, maintain data integrity, and ensure the reliable operation of telemedicine services.
This section delves into the specific security risks associated with these devices and Artikels a robust approach to their secure deployment and ongoing management.
The inherent vulnerabilities of IoMT devices stem from their design, deployment, and management practices. Many devices lack robust security features from the outset, while others suffer from inadequate updates and patch management. This vulnerability landscape extends across a range of device types, each with its own unique set of risks.
Security Risks Associated with IoMT Devices
A variety of security risks are associated with IoMT devices used in telemedicine. These include unauthorized access to patient data through vulnerabilities in device firmware or communication protocols, data breaches due to weak authentication mechanisms, and the potential for malicious actors to manipulate device functionality, leading to inaccurate readings or compromised patient safety. For instance, a compromised insulin pump could deliver incorrect dosages, while a compromised wearable fitness tracker might leak personal health information.
Further risks include the lack of standardized security protocols across different devices and manufacturers, hindering interoperability and creating security gaps. Finally, the sheer volume and diversity of IoMT devices deployed in a telemedicine environment makes comprehensive security management a complex undertaking.
Secure Deployment and Management of IoMT Devices
A robust, multi-layered approach is necessary for the secure deployment and management of IoMT devices. This involves a step-by-step procedure encompassing several key phases:
- Device Selection and Vetting: Prioritize devices from reputable manufacturers with a proven track record of security. Thoroughly review the device’s security specifications, including encryption protocols, authentication mechanisms, and firmware update capabilities. Conduct vulnerability assessments before deployment.
- Network Segmentation: Isolate IoMT devices from other network segments to limit the impact of a potential breach. This can involve the use of dedicated VLANs or VPNs.
- Secure Configuration: Implement strong default passwords, disable unnecessary services, and enable appropriate security features such as firewalls and intrusion detection systems. Regularly review and update device configurations as needed.
- Firmware Updates and Patch Management: Establish a systematic process for applying firmware updates and security patches promptly. This requires close monitoring of security advisories from manufacturers and the implementation of automated update mechanisms where possible.
- Data Encryption: Encrypt all data transmitted between IoMT devices and the telemedicine platform, both in transit and at rest. Use strong encryption algorithms and protocols.
- Access Control: Implement robust access control mechanisms to restrict access to IoMT devices and patient data based on the principle of least privilege. Utilize role-based access control (RBAC) to manage user permissions effectively.
- Regular Security Audits and Penetration Testing: Conduct regular security audits and penetration testing to identify and address vulnerabilities proactively. These assessments should cover both the devices themselves and the entire telemedicine infrastructure.
Implementing Secure Boot Processes and Secure Element Technologies, Securing iomt solutions for telemedicine
Secure boot processes ensure that only authorized firmware is loaded onto the device, preventing malicious code from being executed. This typically involves verifying the digital signature of the firmware before execution. Secure elements, such as hardware security modules (HSMs), provide a tamper-resistant environment for storing sensitive cryptographic keys and performing cryptographic operations. They significantly enhance the security of authentication, data encryption, and other security-critical functions.
For example, a secure element could be used to store and manage the cryptographic keys used to encrypt patient data on a wearable device, preventing unauthorized access even if the device itself is compromised. The integration of these technologies into the design and manufacturing process of IoMT devices is paramount for robust security.
Regulatory Compliance and Security Standards: Securing Iomt Solutions For Telemedicine

Source: cloudfront.net
Navigating the complex landscape of telemedicine IoT security requires a deep understanding of relevant regulations and standards. Failure to comply can lead to significant legal and financial repercussions, not to mention damage to reputation and patient trust. This section will Artikel key regulatory requirements and security standards, offering best practices for achieving compliance in the context of telemedicine IoT deployments.The regulatory environment surrounding healthcare data is incredibly stringent, and rightfully so.
Patient information is highly sensitive, and breaches can have devastating consequences. Therefore, robust security measures are not just good practice – they’re a legal necessity.
Key Regulatory Requirements and Security Standards
Several key regulations and standards directly impact the security of telemedicine IoT solutions. Understanding these frameworks is crucial for building and deploying secure systems. These regulations often overlap, requiring a holistic approach to compliance.
- HIPAA (Health Insurance Portability and Accountability Act): In the United States, HIPAA dictates how protected health information (PHI) must be handled, stored, and transmitted. This includes stringent requirements for data encryption, access control, and audit trails, all crucial aspects of securing telemedicine IoT devices and data flows. Non-compliance can result in hefty fines and legal action.
- GDPR (General Data Protection Regulation): Within the European Union, the GDPR establishes a comprehensive framework for protecting personal data. Similar to HIPAA, it mandates robust security measures, including data minimization, consent management, and the right to be forgotten. The GDPR applies to any organization processing personal data of EU residents, regardless of the organization’s location.
- NIST Cybersecurity Framework: While not a regulation itself, the NIST Cybersecurity Framework provides a voluntary framework for managing and reducing cybersecurity risk. Its five functions – Identify, Protect, Detect, Respond, and Recover – offer a comprehensive approach to building a robust security posture, applicable to telemedicine IoT solutions. Many organizations use NIST as a benchmark for their security practices, even if not legally required.
- ISO 27001: This international standard specifies requirements for establishing, implementing, maintaining, and continually improving an information security management system (ISMS). Achieving ISO 27001 certification demonstrates a commitment to robust security practices, building trust with patients and stakeholders.
Best Practices for Compliance
Implementing effective security measures requires a proactive and multi-faceted approach. Here are some best practices for complying with relevant regulations and standards:
- Data Encryption: Encrypt both data at rest and in transit using strong encryption algorithms to protect against unauthorized access.
- Access Control: Implement role-based access control (RBAC) to limit access to sensitive data based on user roles and responsibilities.
- Regular Security Audits and Penetration Testing: Conduct regular security assessments to identify vulnerabilities and ensure compliance with regulations.
- Incident Response Plan: Develop and regularly test an incident response plan to effectively manage security breaches.
- Employee Training: Educate employees on security best practices and the importance of data protection.
- Vendor Risk Management: Carefully vet third-party vendors and ensure they meet the same security standards as your organization.
- Data Minimization: Collect only the necessary data and retain it only for as long as needed.
Approaches to Achieving Compliance
Organizations can adopt various strategies to achieve compliance with these regulations and standards. The optimal approach depends on factors such as the organization’s size, resources, and risk tolerance.
Securing IoMT solutions for telemedicine is crucial for patient data privacy. This is especially important as AI integration expands, like with the recent news that Nuance integrates generative AI scribe with Epic EHRs , highlighting the need for robust security measures. Strong cybersecurity practices are essential to protect sensitive health information transmitted during virtual consultations and prevent breaches within these increasingly sophisticated systems.
- In-house Development and Management: Organizations with sufficient resources and expertise can develop and manage their own security infrastructure and processes.
- Outsourcing to Managed Security Service Providers (MSSPs): MSSPs offer a range of security services, including security monitoring, incident response, and compliance support. This can be a cost-effective solution for organizations lacking in-house expertise.
- Hybrid Approach: A combination of in-house capabilities and outsourced services can provide a flexible and scalable solution.
- Adopting Pre-built Compliant Solutions: Utilizing telemedicine platforms and IoT devices that are already designed and certified to meet relevant standards can significantly simplify the compliance process.
User Authentication and Authorization in Telemedicine IoT Systems
Securing access to sensitive patient data in telemedicine systems reliant on IoT devices is paramount. A robust authentication and authorization framework is crucial to prevent unauthorized access and maintain patient privacy and data integrity. This requires a multi-layered approach combining strong authentication methods with granular access control mechanisms.Effective user authentication and authorization ensures only authorized personnel can access patient data and control medical devices.
This prevents data breaches, maintains patient confidentiality, and ensures the integrity of the telemedicine system. Failing to implement proper security measures can lead to serious legal and ethical repercussions.
Multi-Factor Authentication and Biometric Authentication Methods
Multi-factor authentication (MFA) significantly enhances security by requiring users to provide multiple forms of verification before granting access. This could involve a combination of something they know (password), something they have (security token), and something they are (biometric scan). For instance, a physician might need to enter a password, receive a one-time code via SMS to their registered mobile phone, and then undergo fingerprint verification before accessing a patient’s electronic health record (EHR) through a connected IoT device.
Biometric authentication, using fingerprints, facial recognition, or iris scans, adds another layer of security by leveraging unique biological traits. However, it’s important to consider privacy implications and ensure compliance with relevant regulations when implementing biometric authentication. The accuracy and reliability of biometric systems also need to be carefully evaluated to prevent false positives or negatives which could compromise security.
Role-Based Access Control (RBAC) Implementation
Role-Based Access Control (RBAC) is a crucial element in managing user permissions. It assigns users to specific roles (e.g., physician, nurse, administrator) each with predefined access rights. A physician might have access to view and modify patient records, while a nurse might only have permission to view certain data points. Administrators, on the other hand, would have broader access for system management.
Implementing RBAC involves defining roles, assigning users to roles, and configuring access control lists (ACLs) to specify what each role can access. This granular control minimizes the risk of data breaches by limiting access to only necessary information based on a user’s assigned role within the system. Regular audits of user roles and permissions are also necessary to maintain security and identify potential vulnerabilities.
Secure User Authentication and Authorization Process Design
A secure telemedicine platform incorporating various IoT devices needs a comprehensive authentication and authorization process. This should include:
- Secure User Registration: A robust registration process that verifies user identities and assigns unique credentials. This could involve email verification, phone number verification, and potentially identity verification using government-issued identification.
- Strong Password Policies: Enforcing complex password requirements (length, character types, regular changes) and potentially using password managers.
- Secure Communication Channels: Utilizing encrypted communication channels (e.g., HTTPS, TLS) to protect data transmitted between IoT devices, the telemedicine platform, and users.
- Device Authentication: Verifying the authenticity of IoT devices connecting to the platform to prevent unauthorized devices from accessing the system. This could involve using digital certificates or other cryptographic techniques.
- Session Management: Implementing secure session management techniques, including session timeouts and automatic logouts, to prevent unauthorized access after a user leaves their device unattended.
- Auditing and Logging: Maintaining detailed logs of all user activities, including login attempts, access to patient data, and device interactions, to facilitate security monitoring and incident response.
This multi-faceted approach ensures a secure and reliable authentication and authorization process, minimizing risks and protecting sensitive patient information within the telemedicine IoT ecosystem.
Incident Response and Security Auditing for Telemedicine IoT
Effective incident response and regular security auditing are critical for maintaining the integrity and confidentiality of telemedicine IoT systems. A proactive approach, combining robust security measures with a well-defined incident response plan and a comprehensive auditing process, is essential to mitigate risks and ensure patient safety and data privacy. Failure to address these areas can lead to significant breaches, compromising sensitive patient information and potentially causing harm.
Incident Response Plan for Telemedicine IoT Security Incidents
A well-defined incident response plan is crucial for minimizing the impact of security incidents. This plan should Artikel clear procedures for identifying, containing, eradicating, and recovering from security breaches involving telemedicine IoT devices. The plan should be regularly tested and updated to reflect changes in the system and emerging threats.
- Preparation: This phase involves establishing baseline security configurations, identifying critical assets, defining roles and responsibilities within the incident response team, and developing communication protocols.
- Identification: This involves detecting security incidents through monitoring systems, security information and event management (SIEM) tools, and intrusion detection systems (IDS). Automated alerts and manual reviews are key to timely identification.
- Containment: Once an incident is identified, immediate actions are needed to isolate affected devices or systems. This may involve disconnecting devices from the network, implementing access controls, or using firewalls to restrict network traffic.
- Eradication: This step focuses on removing the root cause of the security incident. This might involve patching vulnerabilities, removing malware, resetting compromised devices, or changing passwords.
- Recovery: After the threat is eradicated, the system needs to be restored to a secure and operational state. This includes restoring data from backups, verifying system integrity, and updating security configurations.
- Post-Incident Activity: A thorough post-incident analysis is crucial to learn from the event and improve future response. This includes documenting the incident, identifying weaknesses in the security posture, and implementing corrective actions to prevent similar incidents.
Security Auditing Process for Telemedicine IoT Systems
Regular security audits are vital for identifying potential threats and vulnerabilities within telemedicine IoT systems. These audits should encompass both technical and administrative aspects, ensuring compliance with relevant regulations and standards. The frequency of audits should be determined based on risk assessment and the criticality of the systems.
- Vulnerability Scanning: Regular vulnerability scans should be conducted to identify weaknesses in software, hardware, and network configurations. Tools like Nessus or OpenVAS can be used to automate this process.
- Penetration Testing: Penetration testing simulates real-world attacks to identify exploitable vulnerabilities. This helps to assess the effectiveness of existing security controls.
- Security Configuration Review: This involves reviewing the security configurations of all telemedicine IoT devices and network infrastructure to ensure they adhere to established security policies and best practices.
- Log Analysis: Analyzing security logs from various sources can help to identify suspicious activities and potential security breaches. This requires effective log management and analysis tools.
- Compliance Audits: Regular audits should be performed to ensure compliance with relevant regulations such as HIPAA, GDPR, and other industry-specific standards.
Security Log Management for Telemedicine IoT Devices
Maintaining comprehensive and accurate security logs is crucial for incident response and security auditing. These logs should contain detailed information about device activities, user actions, and network traffic. Appropriate retention policies must be established and adhered to, balancing the need for data retention with storage capacity and compliance requirements.
The information logged should include timestamps, user IDs, device IDs, event types (login attempts, data access, system changes), source and destination IP addresses, and any error messages. Retention periods should comply with relevant regulations and should be long enough to support investigations but not excessively long to manage storage.
For example, HIPAA requires maintaining audit trails for a minimum of six years. However, a longer retention period might be necessary depending on the specific requirements and risk profile of the telemedicine system. Regular log rotation and archiving procedures are crucial to ensure efficient log management and data integrity.
Closing Notes
Securing telemedicine IoT solutions is a continuous journey, not a destination. The evolving threat landscape necessitates constant vigilance and adaptation. By implementing the strategies and best practices Artikeld in this post, healthcare providers can significantly reduce their risk profile and ensure the confidentiality, integrity, and availability of patient data. Remember, prioritizing security isn’t just a regulatory requirement; it’s a fundamental ethical responsibility in the delivery of modern healthcare.
Staying informed and proactive is key to building a secure and trustworthy telemedicine future.
Key Questions Answered
What are the biggest threats to telemedicine IoT security?
Major threats include unauthorized access, data breaches, malware infections, denial-of-service attacks, and vulnerabilities in IoT devices themselves.
How can I ensure my telemedicine devices are regularly updated?
Implement a robust patch management system that automatically updates firmware and software on all connected devices. Regular security audits are also crucial.
What is the role of employee training in telemedicine security?
Employee training is vital. Staff should be educated on security protocols, phishing awareness, and best practices for handling sensitive patient data.
How do I choose a secure cloud storage solution for telemedicine data?
Look for solutions with strong encryption, access controls, and compliance certifications (like HIPAA or GDPR). Check their security audits and incident response plans.