Healthcare Burnout A Crisis, Says CDC
Calling healthcare burnout a crisis is an understatement cdc officials w – Calling healthcare burnout a crisis is an understatement, CDC officials warn, and it’s a statement that should send shivers down our spines. We’re not just talking about stress; we’re talking about a systemic collapse threatening the very fabric of our healthcare system. The CDC’s declaration isn’t just a headline; it’s a wake-up call, highlighting the devastating impact of burnout on healthcare professionals and, ultimately, on patient care.
This isn’t just a problem; it’s a full-blown emergency demanding immediate and comprehensive action.
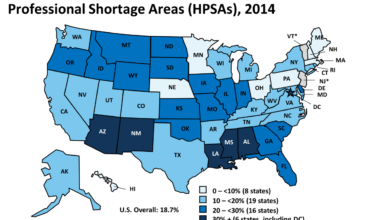
The sheer scale of the crisis is staggering. Years of understaffing, crushing workloads, and a lack of adequate support systems have pushed healthcare workers to their breaking point. The consequences are far-reaching, impacting not only individual well-being but also the quality and safety of patient care. From increased medical errors to compromised efficiency, the ripple effects of burnout are felt throughout the entire healthcare system.
The CDC’s Statement

Source: statnews.com
The Centers for Disease Control and Prevention (CDC) declaring healthcare worker burnout a crisis is a monumental shift in how we perceive and address this pervasive problem. It moves beyond acknowledging burnout as a mere occupational hazard and elevates it to a public health emergency demanding immediate and comprehensive action. This isn’t just about employee morale; it’s about patient safety, healthcare system stability, and the overall well-being of our communities.The significance of the CDC’s statement lies in its far-reaching implications.
By officially labeling burnout a crisis, the CDC underscores the severity and widespread nature of the problem. This isn’t a localized issue affecting a few hospitals; it’s a systemic failure impacting the entire healthcare workforce. The consequences of underestimating this severity are potentially catastrophic. We risk exacerbating existing staff shortages, compromising the quality of care, increasing medical errors, and ultimately, jeopardizing the health and safety of patients.
The ripple effects extend to increased healthcare costs, reduced access to care, and a decline in the overall effectiveness of our healthcare systems.
Impact on Public Perception and Policy
The CDC’s declaration dramatically alters public perception of healthcare worker burnout. Previously, burnout might have been seen as a personal failing or simply an unavoidable consequence of a demanding profession. Now, it’s recognized as a systemic problem requiring collective action. This shift in perception can influence public opinion and encourage greater support for policies aimed at addressing burnout.
For example, the statement could lead to increased funding for mental health resources for healthcare workers, improvements in workplace conditions, and stronger regulations to mitigate burnout-inducing factors. Furthermore, the statement could influence public discourse, leading to greater empathy and understanding of the challenges faced by healthcare professionals. This heightened awareness could inspire individual and community-level initiatives aimed at supporting healthcare workers and improving their well-being.
Comparison to Previous Assessments
Prior to the CDC’s crisis declaration, assessments of healthcare worker well-being often focused on individual coping mechanisms or isolated workplace improvements. While acknowledging the prevalence of burnout, these assessments often lacked the urgency and comprehensive approach now advocated by the CDC. Previous reports might have highlighted high rates of stress, depression, and anxiety among healthcare professionals, but they didn’t necessarily frame these findings within the context of a full-blown crisis.
The CDC’s statement represents a significant escalation in the official recognition of the problem’s magnitude and the urgent need for systemic change. This shift in perspective reflects a growing understanding of the interconnectedness of individual well-being, workplace conditions, and the overall functioning of the healthcare system. The previous approach of treating burnout as a series of isolated problems is now being replaced by a more holistic approach that addresses the systemic issues contributing to the crisis.
Seriously, calling healthcare burnout a crisis is an understatement – CDC officials weren’t kidding! The sheer exhaustion is fueling a massive staffing shortage, and it’s not just anecdotal; as this article from Santenews highlights, healthcare executives say talent acquisition labor shortages are a major business risk. This means the burnout crisis isn’t just impacting individual well-being, it’s crippling the entire system, further emphasizing the urgency of the situation.
Contributing Factors to the Burnout Crisis
The healthcare burnout crisis isn’t simply a matter of overworked individuals; it’s a systemic issue fueled by a complex interplay of factors. Understanding these contributing elements is crucial to developing effective and sustainable solutions. Ignoring these factors will only exacerbate the problem, leading to further deterioration of healthcare quality and a worsening shortage of qualified professionals.
The following table summarizes key factors contributing to healthcare professional burnout, their impact, and potential solutions. It’s important to remember that these factors often interact and influence each other, creating a multifaceted challenge.
| Factor | Description | Impact | Potential Solutions |
|---|---|---|---|
| Administrative Burdens | Excessive paperwork, complex billing processes, electronic health record (EHR) system inefficiencies, and regulatory compliance demands. | Reduces time spent with patients, increases stress and frustration, contributes to feelings of inefficiency and lack of control. | Streamline administrative processes, invest in user-friendly EHR systems, reduce unnecessary paperwork, delegate administrative tasks to support staff. |
| Long Working Hours | Extended shifts, on-call duties, and inadequate time for rest and recovery. | Leads to physical and mental exhaustion, increased risk of medical errors, impaired decision-making, and strained personal relationships. | Implement policies limiting working hours, provide adequate staffing levels to avoid excessive overtime, promote a culture that values work-life balance. |
| Inadequate Staffing Levels | Insufficient number of healthcare professionals to meet patient demand. | Increased workload for existing staff, compromised patient care, heightened stress and risk of burnout, potential for increased medical errors. | Increase recruitment and retention efforts, improve compensation and benefits, offer flexible scheduling options, provide adequate training and support. |
| Workplace Culture | Lack of support from colleagues and supervisors, toxic work environments characterized by bullying, harassment, or lack of recognition. | Damages morale, fosters feelings of isolation and inadequacy, negatively impacts mental health, increases turnover rates. | Promote a culture of respect and collaboration, implement robust anti-bullying and harassment policies, provide regular feedback and recognition, encourage teamwork and open communication. |
| Lack of Support Systems | Inadequate access to mental health services, insufficient resources for stress management and well-being initiatives. | Increases vulnerability to burnout, delays seeking help for mental health concerns, exacerbates feelings of isolation and helplessness. | Provide access to mental health services, offer stress management programs, implement employee assistance programs (EAPs), create supportive peer networks. |
Impact of Administrative Burdens, Long Working Hours, and Inadequate Staffing Levels on Burnout
The combined effect of these three factors is particularly devastating. Administrative burdens steal valuable time away from direct patient care, leaving healthcare professionals feeling frustrated and undervalued. Long working hours, often coupled with inadequate staffing, exacerbate this feeling, leading to physical and mental exhaustion. The constant pressure to do more with less creates a vicious cycle of stress, impacting both professional performance and personal well-being.
For example, a study published in the
-Journal of the American Medical Association* found a strong correlation between long working hours and increased risk of burnout among physicians.
The Role of Workplace Culture and Support Systems in Mitigating Burnout
A positive and supportive workplace culture is paramount in combating burnout. When healthcare professionals feel valued, respected, and supported by their colleagues and supervisors, they are better equipped to cope with the inherent stresses of their profession. Robust support systems, including access to mental health services and stress management programs, provide crucial resources for managing burnout and promoting well-being.
Hospitals and clinics that prioritize employee well-being often experience lower turnover rates and improved patient care.
Innovative Approaches to Address Contributing Factors
Innovative solutions are needed to address the multifaceted nature of this crisis. Examples include implementing telehealth technologies to reduce administrative burdens and improve access to care, utilizing AI-powered tools to automate tasks and streamline workflows, and fostering mentorship programs to provide support and guidance to new professionals. Investing in leadership training to cultivate positive workplace cultures and promoting flexible work arrangements can also contribute to reducing burnout.
For instance, some hospitals are experimenting with four-day workweeks to improve work-life balance and reduce fatigue among staff.
Impact on Healthcare Systems and Patient Care
Healthcare burnout isn’t just a problem for individual professionals; it’s a systemic crisis that significantly impacts the quality of patient care and the overall efficiency of healthcare systems. The widespread exhaustion and cynicism among healthcare workers have far-reaching consequences, affecting everything from diagnostic accuracy to patient safety and ultimately, the financial sustainability of healthcare organizations.The effects of burnout ripple throughout the healthcare system.
When healthcare professionals are perpetually stressed and overwhelmed, their ability to provide optimal care is compromised. This isn’t just about a slight decrease in efficiency; it’s about a potential increase in medical errors, delayed diagnoses, and a decline in the overall patient experience. The emotional toll on caregivers also leads to reduced empathy and compassion, impacting the human connection so crucial to effective healthcare.
Honestly, calling healthcare burnout a crisis is an understatement – CDC officials warned us, and it’s only getting worse. One potential solution, highlighted in a fascinating study widespread digital twins healthcare , explores using digital twins to improve efficiency and reduce workload. Ultimately, though, addressing the burnout crisis requires a multi-pronged approach, going far beyond technological fixes alone.
Reduced Quality of Patient Care
Burnout leads to a demonstrable decline in the quality of patient care. Studies have shown a direct correlation between high burnout rates and increased medical errors, longer hospital stays, and higher rates of patient readmission. For example, fatigued nurses may be more prone to medication errors, while overworked physicians might miss subtle signs of a worsening condition. This diminished capacity for attention to detail directly impacts patient safety and outcomes.
Seriously, calling healthcare burnout a crisis is an understatement – the CDC officials weren’t kidding. The recent new york state nurse strike NYSNA Montefiore Mount Sinai perfectly illustrates the breaking point; exhausted nurses demanding better staffing and working conditions. It’s a stark reminder of how deeply rooted this problem is, and why we need immediate, systemic change to prevent further collapse of our healthcare system.
Furthermore, the emotional exhaustion experienced by healthcare professionals can lead to reduced empathy and communication with patients, impacting the overall patient experience and their trust in the healthcare system.
Impact on Healthcare System Efficiency and Costs
Burnout significantly impacts healthcare system efficiency and contributes to escalating costs. High turnover rates, a direct consequence of burnout, require substantial investment in recruitment and training of new staff. This constant cycle of hiring and onboarding is costly and disrupts the continuity of care. Moreover, burnout can lead to increased absenteeism and presenteeism (being physically present but mentally checked out), both of which decrease productivity and efficiency.
The increased medical errors associated with burnout also translate to higher healthcare costs due to extended hospital stays, additional treatments, and potential legal ramifications.
Correlation Between Burnout and Adverse Patient Outcomes
Numerous studies have established a clear link between high burnout rates among healthcare professionals and increased medical errors, adverse patient outcomes, and even increased mortality rates. For instance, a study published in theJournal of the American Medical Association* found a strong correlation between physician burnout and a higher risk of patient mortality. Similarly, research has shown that burnout among nurses is associated with an increased incidence of medication errors and patient falls.
These findings highlight the critical need to address burnout not just for the well-being of healthcare workers, but also to improve patient safety and overall healthcare quality.
Burnout Across Healthcare Professions
The impact of burnout varies across different healthcare professions, although the underlying issues are often similar.
| Profession | Effects of Burnout |
|---|---|
| Physicians | Increased medical errors, diagnostic delays, reduced patient satisfaction, higher rates of depression and substance abuse, decreased job satisfaction, potential for early retirement. |
| Nurses | Increased medication errors, patient falls, increased risk of infections, compassion fatigue, high turnover rates, physical and emotional exhaustion. |
| Support Staff | Increased stress levels, higher rates of absenteeism, reduced morale, decreased efficiency, potential for burnout to affect patient care indirectly through reduced support for clinical staff. |
Strategies for Addressing the Crisis
Healthcare worker burnout is no longer a problem; it’s a full-blown crisis demanding immediate and comprehensive action. Simply acknowledging the severity isn’t enough; we need concrete strategies to mitigate its devastating effects on both healthcare professionals and the patients they serve. This requires a multi-pronged approach focusing on systemic changes, individual support, and improved team dynamics.
A comprehensive plan must address burnout at multiple levels, from individual well-being to organizational culture. This means investing in resources, implementing evidence-based interventions, and fostering a culture of support and collaboration. Ignoring any one of these elements will render the others ineffective. The goal is to create a sustainable system that prioritizes the well-being of healthcare workers while simultaneously enhancing the quality of patient care.
Successful Interventions to Reduce Burnout and Improve Well-being
Numerous studies have demonstrated the effectiveness of specific interventions in reducing burnout and improving the well-being of healthcare professionals. These interventions often involve a combination of approaches tailored to individual needs and organizational contexts. For example, mindfulness-based stress reduction programs have shown significant reductions in burnout symptoms among nurses. Similarly, access to employee assistance programs (EAPs) providing counseling and mental health services can significantly improve mental health outcomes.
Furthermore, providing opportunities for professional development and career advancement can boost morale and job satisfaction, indirectly reducing burnout.
Creating Supportive Work Environments
A supportive work environment is crucial for mitigating burnout. This goes beyond simply providing adequate staffing levels; it involves fostering a culture of respect, collaboration, and open communication. For instance, implementing fair scheduling practices that minimize overtime and provide adequate time off can significantly reduce stress. Creating opportunities for social interaction and team-building activities can also foster a sense of community and belonging, which is vital for combating feelings of isolation and overwhelm.
Additionally, actively promoting work-life balance initiatives, such as flexible work arrangements and on-site childcare facilities, can help alleviate stress outside of the workplace and positively impact overall well-being. Leadership plays a critical role in establishing and maintaining a supportive work environment. Leaders who model healthy behaviors, actively listen to their staff’s concerns, and provide constructive feedback contribute significantly to a positive work culture.
Strategies for Improving Communication and Collaboration Among Healthcare Teams
Effective communication and collaboration are fundamental to a healthy and productive healthcare team. Poor communication can exacerbate stress and contribute to burnout. Implementing clear communication protocols, such as standardized handoffs and regular team meetings, can improve efficiency and reduce misunderstandings. Investing in training programs that focus on conflict resolution and teamwork skills can equip healthcare professionals with the tools they need to navigate challenging situations effectively.
Utilizing technology, such as secure messaging platforms and electronic health records, can streamline communication and reduce administrative burden. Furthermore, creating a culture of open communication, where staff feel comfortable voicing their concerns and suggestions without fear of reprisal, is essential for fostering a collaborative and supportive work environment. This might involve establishing regular feedback mechanisms, such as anonymous surveys or suggestion boxes, to gather input from staff and address their concerns promptly.
A hospital in California, for example, implemented a peer-support program where experienced nurses mentored new hires, resulting in a significant reduction in staff turnover and improved team cohesion.
Long-Term Solutions and Prevention

Source: cloudfront.net
The current healthcare burnout crisis isn’t just a temporary setback; it’s a systemic issue demanding long-term, sustainable solutions. Ignoring the need for preventative measures will only lead to a cyclical pattern of crisis and insufficient response. We need a fundamental shift in how we approach healthcare worker well-being, moving beyond reactive measures to proactive strategies that foster a healthier and more sustainable work environment.
This requires a multi-pronged approach involving individual responsibility, institutional changes, and crucial policy reforms.Addressing healthcare burnout requires a comprehensive strategy focusing on prevention and sustainable solutions. Simply addressing the immediate symptoms without tackling the root causes will only provide temporary relief. We need to cultivate a culture of well-being within healthcare systems, promoting work-life balance, and empowering healthcare professionals to prioritize their mental and physical health.
This shift demands a collaborative effort from individuals, institutions, and policymakers, all working towards a common goal of a thriving healthcare workforce.
Systemic Policy Changes to Mitigate Burnout
Systemic issues within healthcare contribute significantly to burnout. These issues are often deeply entrenched and require significant policy changes to address effectively. For instance, excessive administrative burden, inadequate staffing levels, and a lack of support for work-life integration are all major contributing factors. Policy changes should focus on reducing administrative tasks, increasing staffing ratios to manageable levels, and providing resources to support healthcare workers’ personal lives.
These changes are not merely beneficial; they are essential for the long-term sustainability of the healthcare system.
Actionable Steps for Individuals, Institutions, and Policymakers
The responsibility for preventing future burnout crises rests on multiple shoulders. Individuals, institutions, and policymakers all have a crucial role to play in creating a healthier and more supportive environment for healthcare workers.
The following steps Artikel actionable strategies:
- Individuals: Prioritize self-care, set boundaries, seek support when needed, engage in stress-reducing activities (e.g., exercise, mindfulness), and advocate for better working conditions.
- Institutions: Implement robust wellness programs, provide access to mental health resources, foster a culture of open communication and feedback, reduce administrative burdens, improve staffing ratios, and offer flexible work arrangements.
- Policymakers: Increase funding for healthcare worker well-being initiatives, implement policies to reduce administrative burdens, mandate minimum staffing ratios, and invest in training programs focused on stress management and resilience.
Investing in Preventative Measures
Investing in preventative measures is not simply a cost; it’s an investment in the future of healthcare. By prioritizing the well-being of healthcare workers, we ensure a more resilient and effective healthcare system. This translates to improved patient care, reduced medical errors, and a more sustainable healthcare workforce. The long-term costs of inaction—increased turnover, recruitment challenges, and compromised patient safety—far outweigh the investment in proactive strategies.
For example, a hospital system that invests in a comprehensive wellness program may see a reduction in staff turnover, leading to cost savings in recruitment and training. Conversely, a system that neglects these issues will likely experience higher turnover rates, impacting the quality of care and driving up costs.
Illustrative Examples of Burnout’s Impact: Calling Healthcare Burnout A Crisis Is An Understatement Cdc Officials W
Source: sma.org
Healthcare burnout isn’t just a feeling; it’s a debilitating condition with far-reaching consequences for both individuals and the healthcare system as a whole. The following examples illustrate the devastating impact burnout can have on the lives of healthcare professionals and the quality of patient care.
Burnout’s Impact on a Healthcare Professional’s Personal and Professional Life, Calling healthcare burnout a crisis is an understatement cdc officials w
Imagine Sarah, a dedicated emergency room nurse working 12-hour shifts, often back-to-back. Initially passionate about her work, she gradually became overwhelmed by the relentless pressure, the emotional toll of witnessing suffering, and the constant understaffing. She started making more mistakes at work, small initially, like forgetting to chart a medication, then more serious, like misinterpreting a vital sign.
Her sleep suffered, leading to irritability and difficulty concentrating, both at work and at home. She withdrew from her family and friends, neglecting her hobbies and personal well-being. Her once vibrant personality dimmed, replaced by exhaustion and cynicism. The once sharp, efficient nurse became hesitant and less confident in her abilities, ultimately impacting her job performance and potentially patient safety.
This isn’t an uncommon scenario; countless healthcare professionals find themselves in similar situations, struggling to maintain a healthy work-life balance amidst the relentless demands of their profession.
Burnout’s Impact on Hospital Efficiency and Patient Outcomes
Consider Dr. David, a highly respected cardiologist who experienced a severe burnout episode after a particularly challenging year marked by high patient mortality and administrative burdens. His exhaustion manifested as decreased attentiveness to detail, leading to a misdiagnosis in a critical case. This resulted in delayed treatment and ultimately worsened the patient’s prognosis. Beyond this individual case, Dr.
David’s burnout also affected his colleagues. His reduced efficiency and negativity impacted team morale and workflow. His colleagues found themselves picking up his slack, leading to increased workload and potential burnout among them as well. The hospital’s overall efficiency decreased, leading to longer wait times for patients, increased medical errors, and ultimately, compromised patient safety and satisfaction. This single case of severe burnout had a ripple effect, impacting the entire hospital system and demonstrating the significant cost of ignoring the problem.
Ending Remarks
The CDC’s declaration that healthcare burnout is a crisis isn’t just a statement; it’s a call to arms. Addressing this issue requires a multi-pronged approach, involving systemic changes, innovative solutions, and a fundamental shift in how we value and support our healthcare heroes. We need to move beyond acknowledging the problem and actively implement strategies that foster healthier work environments, reduce burnout rates, and ensure the sustainability of our healthcare system.
The future of healthcare depends on it.
Answers to Common Questions
What specific support systems are lacking in healthcare settings that contribute to burnout?
Many healthcare settings lack adequate mental health resources, mentorship programs, and opportunities for professional development, all of which contribute to burnout.
How does burnout specifically impact patient safety?
Burnout leads to increased medical errors, decreased attention to detail, and reduced empathy, all of which negatively affect patient safety and outcomes.
Are there any legal ramifications for hospitals failing to address healthcare worker burnout?
While not explicitly stated in law, hospitals failing to address burnout could face lawsuits related to negligence or substandard care stemming from burnout-related errors.
What role do insurance companies play in addressing burnout?
Insurance companies can play a significant role by covering mental health services for healthcare professionals and incentivizing hospitals to implement burnout prevention programs.