Primary Care Providers Say Field Is Crumbling
Primary care providers say field is crumbling – Primary care providers say the field is crumbling, and it’s a crisis unfolding right before our eyes. Doctors are burning out, administrative burdens are crushing them, and patients are facing longer wait times and reduced access to care. This isn’t just a problem for doctors; it’s a systemic issue that threatens the health and well-being of entire communities. We’ll delve into the factors driving this collapse, explore the impact on patients, and examine potential solutions to prevent a complete breakdown of our primary care system.
From skyrocketing burnout rates and crippling administrative tasks to inadequate reimbursement and a shrinking workforce, the challenges facing primary care are immense. The consequences are far-reaching, impacting not only the physicians themselves but also the quality and accessibility of care for patients, particularly vulnerable populations. This post aims to shed light on this critical situation, examining the root causes, exploring potential solutions, and offering a glimpse into the future of primary care.
The Current State of Primary Care

Source: theatlantic.com
The narrative surrounding primary care is often bleak. We hear frequent pronouncements that the field is crumbling, a system overwhelmed and on the verge of collapse. While the situation is undoubtedly challenging, it’s crucial to move beyond the dramatic pronouncements and analyze the specific factors contributing to this perceived crisis. Understanding these challenges is the first step towards implementing effective solutions.
The core issue is a complex interplay of factors impacting both primary care providers (PCPs) and their patients. Burnout among PCPs is rampant, leading to physician shortages and reduced access to care. Simultaneously, the increasing complexity of chronic disease management and the rising cost of healthcare create a perfect storm that threatens the sustainability of primary care as we know it.
Challenges Faced by Primary Care Providers
Primary care physicians face an unrelenting barrage of administrative burdens, including complex billing processes, electronic health record (EHR) documentation requirements, and increasing regulatory compliance demands. These tasks often consume a significant portion of their workday, diverting time and energy away from direct patient care. Beyond the administrative hurdles, PCPs struggle with inadequate reimbursement rates, leading to financial strain and impacting their ability to invest in their practices and staff.
The sheer volume of patients coupled with the increasing complexity of their needs contributes significantly to burnout and early retirement. This shortage of PCPs, in turn, creates longer wait times for appointments and decreased access to timely, quality care for patients.
Factors Contributing to the Crumbling of Primary Care
The “crumbling” of primary care is not a singular event but a gradual erosion driven by multiple, interconnected factors. These factors include unsustainable reimbursement models that fail to adequately compensate PCPs for the comprehensive care they provide, a growing administrative burden that diverts time from patient care, and a significant shortage of PCPs due to burnout and retirement. The increasing complexity of patient needs, driven by the rising prevalence of chronic diseases, further exacerbates the situation.
Finally, the lack of sufficient investment in primary care infrastructure and workforce development perpetuates the cycle.
Impact on Patient Care
The challenges faced by PCPs directly translate into negative impacts on patient care. Increased wait times for appointments lead to delayed diagnoses and treatment, potentially worsening patient outcomes. Burnout among PCPs can result in reduced empathy and compassion, negatively affecting the patient-provider relationship. Limited access to PCPs can force patients to rely on more expensive and less coordinated care in emergency rooms or specialist offices.
Furthermore, the administrative burden on PCPs may result in less time spent on preventative care, leading to a rise in preventable hospitalizations and chronic disease complications.
Factors Impacting Primary Care: A Summary
| Factor | Impact on Providers | Impact on Patients | Potential Solutions |
|---|---|---|---|
| Inadequate Reimbursement | Financial strain, difficulty hiring staff, reduced ability to invest in practice | Limited access to care, longer wait times, potentially lower quality of care | Increased reimbursement rates, value-based payment models |
| Administrative Burden | Burnout, reduced time for patient care, decreased job satisfaction | Longer wait times, less personalized care, potential for medical errors due to rushed appointments | Streamlined EHR systems, reduced regulatory burden, increased administrative support |
| Physician Shortage | Increased workload, burnout, decreased job satisfaction | Limited access to care, longer wait times, potential delays in diagnosis and treatment | Increased funding for medical education, loan forgiveness programs, improved working conditions |
| Increasing Complexity of Patient Needs | Increased workload, stress, burnout | Potential for delayed or fragmented care, increased healthcare costs | Improved care coordination, investment in chronic disease management programs, increased use of telehealth |
Burnout and Workforce Shortages
The crumbling foundation of primary care isn’t just about funding or regulations; it’s deeply rooted in the well-being of its practitioners and the sheer lack of people willing or able to fill the ever-growing need for care. High rates of burnout among physicians, coupled with a significant shortage of primary care providers, create a perfect storm threatening the accessibility and quality of healthcare for millions.The current crisis is a culmination of long-standing issues, exacerbated by recent pressures.
Burnout among primary care physicians is significantly higher than in other medical specialties, leading to decreased job satisfaction, increased errors, and ultimately, attrition from the field. This, in turn, fuels the already critical shortage of primary care providers, creating a vicious cycle that impacts patient care and the overall healthcare system.
High Rates of Physician Burnout
Primary care physicians face immense pressure from administrative burdens, increasing patient loads, and the emotional toll of managing complex patient needs. Studies consistently show burnout rates exceeding 50% in primary care, significantly impacting their mental and physical health. The constant pressure to meet performance metrics, coupled with long hours and inadequate support systems, contributes to this alarming statistic.
So many primary care providers are saying the field is crumbling under the weight of administrative burdens and low reimbursements. It’s interesting to see how companies like Humana are trying to address this, like with their partnership opening humana centerwell primary care centers walmart , which might offer a different model. But even these innovative approaches can’t fully solve the underlying issues causing primary care providers to feel overwhelmed and burnt out.
This isn’t simply a matter of personal resilience; systemic issues within the healthcare system are directly responsible for creating an unsustainable work environment. For example, the increasing complexity of electronic health records (EHRs) adds significant administrative burden, taking time away from direct patient care and increasing frustration. The resulting stress contributes significantly to burnout.
Reasons for Primary Care Provider Shortages
Several factors contribute to the shortage of primary care providers. Firstly, the medical education system has historically favored lucrative specialties like surgery and cardiology, leading to fewer medical students choosing primary care. Secondly, the lower reimbursement rates for primary care services compared to specialty care make it less financially attractive for physicians. Thirdly, the increasing administrative burden and bureaucratic complexities associated with modern healthcare practices contribute to physician dissatisfaction and burnout, driving many to leave the field or choose alternative career paths.
Finally, the aging population of current primary care physicians is nearing retirement without a sufficient pipeline of replacements. The current trend demonstrates a clear gap between the growing demand for primary care services and the dwindling supply of providers.
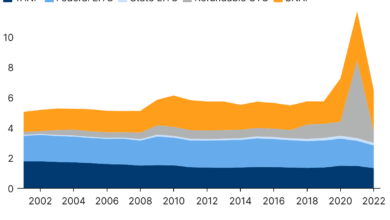
Historical Trends in the Primary Care Workforce
Historically, primary care has always faced challenges in attracting and retaining physicians. However, the current situation represents an unprecedented crisis. While there have been periods of fluctuation in the number of primary care physicians, the current rate of burnout and the lack of new entrants into the field are far exceeding historical trends. For instance, the number of primary care physicians per capita has been steadily declining in many developed countries over the past decade, while the demand for their services continues to grow due to an aging population and increased prevalence of chronic diseases.
This trend suggests a worsening situation unless significant changes are implemented.
A Potential Recruitment Strategy, Primary care providers say field is crumbling
Addressing the primary care provider shortage requires a multi-pronged approach. A comprehensive recruitment strategy should include:
- Increasing financial incentives for primary care physicians through improved reimbursement rates and loan forgiveness programs.
- Reducing administrative burdens by simplifying billing processes and improving EHR systems.
- Investing in mentorship programs and fostering a supportive work environment to reduce burnout and improve job satisfaction.
- Promoting primary care as a rewarding and fulfilling career path through targeted outreach to medical students and residents.
- Expanding the scope of practice for other healthcare professionals, such as nurse practitioners and physician assistants, to alleviate some of the workload on physicians.
This strategy needs to be implemented at both the national and local levels, involving collaboration between government agencies, medical schools, and healthcare organizations. The success of such a strategy hinges on a systemic shift in prioritizing primary care, acknowledging its vital role in the healthcare system, and investing in the well-being of its practitioners.
Administrative Burden and Reimbursement Issues
Source: co.uk
The crumbling foundation of primary care isn’t just about burnout and staffing shortages; it’s deeply intertwined with the crushing weight of administrative tasks and inadequate reimbursement models. These factors significantly impact providers’ time, compensation, and ultimately, their ability to deliver quality patient care. The sheer volume of paperwork, coding, and billing processes consumes precious hours that could be spent directly with patients.
This administrative burden, coupled with reimbursement rates that often fail to cover the actual cost of care, creates a perfect storm pushing many providers to the brink.The administrative tasks that dominate a primary care provider’s day are numerous and often frustratingly inefficient. Consider the time spent on prior authorizations for medications, navigating complex electronic health record (EHR) systems, completing endless forms for insurance companies, and managing billing and coding complexities.
These tasks often require specialized knowledge and training, diverting attention from the core mission of providing patient care. For example, a physician might spend an hour each day simply managing prior authorizations, time that could have been used for patient consultations or preventative care. The cumulative effect is a significant reduction in direct patient care time, impacting both the quality and quantity of services offered.
Examples of Reimbursement Models’ Impact on Provider Compensation and Practice Viability
Current reimbursement models, often based on fee-for-service structures, frequently fall short of adequately compensating primary care providers for the comprehensive care they provide. Many insurance plans reimburse at rates that don’t cover the true cost of providing services, including staffing, overhead, and malpractice insurance. This results in practices struggling to stay afloat financially, forcing them to reduce staff, limit services, or even close altogether.
For instance, a small primary care practice might find that the reimbursement for a routine check-up is significantly less than the actual cost of providing that service, including the physician’s time, nurse’s time, lab tests, and administrative overhead. This financial strain can lead to reduced provider salaries, limited investment in technology and staff training, and ultimately, compromised patient care.
The Relationship Between Administrative Burden and Provider Burnout
The constant pressure of administrative tasks, combined with inadequate compensation, is a major driver of physician burnout. The endless cycle of paperwork, billing issues, and navigating complex insurance systems creates a sense of frustration and overwhelm. This administrative burden contributes significantly to feelings of exhaustion, cynicism, and a diminished sense of personal accomplishment. Studies have consistently shown a strong correlation between administrative burden and burnout among primary care physicians, highlighting the need for systemic changes to alleviate this pressure.
The constant struggle to balance administrative duties with patient care leads to decreased job satisfaction and increased rates of physician turnover, further exacerbating the primary care crisis.
Potential Policy Changes to Alleviate Administrative Burdens
Addressing the administrative burden requires significant policy changes at both the state and federal levels. Several potential solutions could significantly improve the situation for primary care providers:
- Simplify prior authorization processes: Streamlining the process for obtaining prior authorizations would free up significant time for providers.
- Increase reimbursement rates for primary care services: Fairer reimbursement rates that reflect the true cost of providing comprehensive care are crucial for practice viability.
- Invest in interoperable EHR systems: Improved EHR systems that facilitate seamless data exchange between providers and payers could reduce administrative workload.
- Implement value-based care models: Shifting from fee-for-service to value-based care models would incentivize providers to focus on quality and outcomes, rather than the volume of services.
- Reduce regulatory burdens: Streamlining regulations and reducing unnecessary paperwork would significantly lessen the administrative burden on providers.
Impact on Patient Access and Outcomes
The crumbling primary care system is having a devastating impact on patient access to care and, consequently, on health outcomes. Fewer primary care physicians mean longer wait times for appointments, reduced availability of preventative services, and delayed diagnoses of serious conditions. This isn’t just an inconvenience; it’s a serious threat to public health.The consequences of limited access to primary care are far-reaching.
Patients face significant hurdles in receiving routine checkups, managing chronic conditions, and accessing timely treatment for acute illnesses. This lack of access disproportionately affects vulnerable populations, leading to worse health outcomes and exacerbating existing health disparities. The ripple effect extends beyond individual patients, impacting the overall health and productivity of communities.
Primary care providers are sounding the alarm; they say the field is crumbling under the weight of administrative burdens and low reimbursement rates. Could advancements like those highlighted in this article on the ai most exciting healthcare technology center connected medicine upmc offer a lifeline? Perhaps AI and connected medicine could alleviate some of the pressures, ultimately helping to shore up this vital sector before it collapses entirely.
Consequences of Limited Access to Care
Reduced access to primary care translates directly into longer wait times for appointments. Imagine a scenario where a patient experiencing chest pains has to wait several weeks to see a doctor, potentially delaying critical diagnosis and treatment of a heart condition. This delay can lead to more severe health complications and increased healthcare costs in the long run. Furthermore, the scarcity of primary care physicians often results in patients resorting to more expensive emergency room visits for non-emergency situations, further burdening the healthcare system.
Impact on Preventative Care and Long-Term Health Outcomes
Preventative care, the cornerstone of a healthy population, suffers greatly under strained primary care systems. Routine screenings for cancer, diabetes, and hypertension are often delayed or forgone altogether due to limited access. This lack of early detection and intervention can lead to more advanced and difficult-to-treat conditions, ultimately resulting in poorer long-term health outcomes and reduced life expectancy.
For example, delayed colon cancer screenings can lead to the discovery of the disease at a later, more aggressive stage, significantly impacting survival rates.
Impact on Vulnerable Populations
Vulnerable populations, including the elderly, low-income individuals, and those with disabilities, are disproportionately affected by the primary care crisis. These individuals often face multiple barriers to accessing healthcare, including lack of transportation, insurance coverage, and language barriers. Limited access to primary care exacerbates these existing challenges, leading to poorer health outcomes and widening health disparities. For instance, a diabetic patient living in a rural area with limited access to primary care may struggle to manage their condition effectively, leading to complications such as blindness or kidney failure.
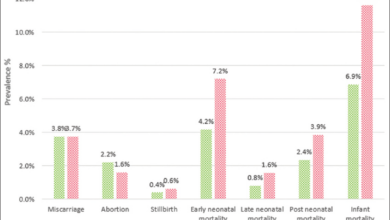
Improved Access and Public Health Metrics
A hypothetical graph illustrating the relationship between improved access to primary care and improved public health metrics would show a positive correlation. The X-axis would represent the level of access to primary care (measured, for example, by the physician-to-patient ratio), and the Y-axis would represent key public health metrics such as life expectancy, rates of chronic disease, and infant mortality.
The graph would show a clear upward trend: as access to primary care improves, these positive public health metrics also improve. For example, an increase in the physician-to-patient ratio from 1:2000 to 1:1000 could be correlated with a noticeable increase in life expectancy and a decrease in preventable deaths from chronic diseases. This illustrates the significant impact that strengthening primary care has on the overall health of a population.
Technological Advancements and Their Role
The rapid evolution of technology is reshaping the landscape of primary care, presenting both unprecedented opportunities and significant challenges. Telehealth and electronic health records (EHRs) are at the forefront of this transformation, profoundly impacting how healthcare is delivered and experienced. While offering potential solutions to the crumbling primary care system, their implementation also brings its own set of complexities.Technological advancements, particularly in telehealth and EHRs, are significantly altering the daily realities of primary care providers and their patients.
The integration of these tools has the potential to streamline workflows, improve access to care, and enhance the quality of patient outcomes. However, it’s crucial to acknowledge the downsides, including increased administrative burden and the potential for exacerbating existing inequalities in healthcare access.
Telehealth Models and Their Effectiveness
Various telehealth models exist, each with its strengths and limitations in addressing access issues. These models range from simple store-and-forward systems (e.g., sending images or test results electronically) to real-time video conferencing, and even remote patient monitoring using wearable devices. The effectiveness of each model depends on factors like the specific needs of the patient population, the technological infrastructure available, and the provider’s comfort level with technology.
For instance, remote patient monitoring is particularly effective for managing chronic conditions like diabetes or hypertension, allowing for continuous data collection and proactive interventions. Video conferencing, on the other hand, is well-suited for routine check-ups or addressing acute issues that don’t require a physical examination. Store-and-forward systems are useful for situations where immediate interaction isn’t necessary, such as the review of radiology images by a specialist.
Comparison of Telehealth Platforms
The choice of telehealth platform significantly impacts both provider workflow and patient experience. The following table Artikels some key pros and cons of different platforms:
| Telehealth Platform | Pros | Cons |
|---|---|---|
| Video Conferencing (e.g., Zoom, Skype) | Real-time interaction, easy to use, widely accessible | Requires reliable internet connection, potential for technical difficulties, privacy concerns |
| Store-and-Forward (e.g., secure messaging systems) | Asynchronous communication, convenient for patients, reduces immediate communication pressure | Can lead to delays in care, less personal interaction, requires robust secure messaging systems |
| Remote Patient Monitoring (RPM) (e.g., wearable devices, connected blood pressure cuffs) | Continuous data collection, proactive interventions, improved chronic disease management | Requires patient engagement and technological literacy, data security concerns, potential for alert fatigue |
Impact of EHRs on Provider Workload and Patient Care
Electronic health records (EHRs) have become ubiquitous in primary care, aiming to streamline documentation and improve care coordination. However, their implementation has also brought about significant challenges. While EHRs offer benefits such as improved data accessibility and reduced paperwork, many providers report increased administrative burden due to the time-consuming nature of data entry and navigating complex systems. This added workload can contribute to physician burnout and potentially detract from time spent directly with patients.
Furthermore, the focus on data entry can sometimes overshadow the crucial elements of patient interaction and relationship-building, potentially impacting the quality of care. The design and usability of different EHR systems also vary widely, influencing their impact on efficiency and user satisfaction. For example, systems with intuitive interfaces and streamlined workflows can mitigate some of the negative impacts, while poorly designed systems can exacerbate the burden.
Potential Solutions and Future Directions

Source: substackcdn.com
The crumbling foundation of primary care demands immediate and multifaceted solutions. We can’t simply patch the cracks; we need to rebuild the entire structure, focusing on sustainable, patient-centered models. This requires a collaborative effort involving policymakers, healthcare administrators, educators, and providers themselves. Only through a comprehensive approach can we hope to revitalize primary care and ensure access to quality healthcare for all.Policy changes are crucial for creating a sustainable primary care system.
These changes need to address the core issues driving the crisis: burnout, administrative burden, and inadequate reimbursement.
Policy Changes to Support Primary Care Providers
Effective policy changes must tackle the root causes of the primary care crisis. Increased funding for primary care services is paramount, providing providers with the resources they need to deliver quality care without being overwhelmed by administrative tasks. This includes direct funding for staffing, technology upgrades, and comprehensive mental health support for providers. Furthermore, policies should streamline the billing and coding processes, reducing the administrative burden that consumes so much of a physician’s time.
This could involve simplifying billing codes, implementing electronic health record (EHR) interoperability standards, and investing in technology that automates administrative tasks. Finally, adjusting reimbursement models to reflect the true cost of providing comprehensive primary care is vital. Value-based care models, which reward providers for positive patient outcomes rather than the volume of services, should be incentivized and widely adopted.
The implementation of these policy changes, particularly in under-resourced communities, could significantly improve access to care and reduce health disparities.
Innovative Models of Primary Care Delivery
The traditional fee-for-service model is unsustainable. Innovative models, such as team-based care, are proving to be more effective and efficient. Team-based care, involving physicians, nurse practitioners, physician assistants, medical assistants, and other healthcare professionals working collaboratively, allows for a more comprehensive and efficient approach to patient care. This model can effectively address the workload issues faced by primary care physicians, ensuring they can dedicate more time to direct patient interaction and less to administrative tasks.
So many primary care providers are saying their field is crumbling under the weight of administrative burdens and low reimbursement rates. It’s no wonder, when you consider the insane complexities of healthcare costs; check out this article on health cost inflation variation price transparency turquoise to see just how messed up pricing can be. This lack of transparency directly impacts the viability of primary care, further accelerating the crisis.
Another example is the rise of direct primary care (DPC) clinics. DPC clinics offer a subscription-based model, providing patients with unlimited access to their primary care provider at a monthly fee. This model eliminates the complexities of insurance billing and allows providers to focus on patient care. These innovative models offer promising pathways to a more sustainable and patient-centered approach to primary care.
For instance, Kaiser Permanente’s integrated system demonstrates the effectiveness of a vertically integrated model, offering comprehensive care from primary care to specialized services under one umbrella, improving coordination and reducing costs.
The Role of Medical Education in Addressing the Crisis
Medical education needs a significant overhaul to address the current crisis. The curriculum should emphasize teamwork, communication skills, and efficient use of technology. Training should incorporate strategies for managing burnout and administrative burdens, equipping future physicians with the tools they need to thrive in the current environment. Furthermore, medical schools should increase the number of primary care residency slots to address the growing shortage of primary care physicians.
Increased emphasis on preventative care and population health management in the curriculum is also critical to address the growing needs of an aging population and the increasing prevalence of chronic diseases. A focus on interprofessional education, fostering collaboration among physicians, nurses, and other healthcare professionals, will improve the efficiency and quality of care delivery.
A Vision for the Future of Primary Care
The future of primary care should be defined by accessible, affordable, and high-quality care delivered through sustainable models. This involves a shift away from the fee-for-service model towards value-based care, incentivizing quality over quantity. Technology will play a crucial role, streamlining administrative tasks, improving communication, and enhancing patient engagement. Team-based care, incorporating the expertise of various healthcare professionals, will be essential.
Finally, a robust support system for primary care providers, addressing burnout and promoting well-being, will be crucial to creating a sustainable and thriving primary care system. This vision necessitates significant investment in primary care infrastructure, training, and technology to ensure that all individuals have access to the high-quality, patient-centered care they deserve.
Last Word: Primary Care Providers Say Field Is Crumbling
The crumbling of primary care is a multifaceted crisis demanding immediate attention. While the challenges are significant, there’s reason for hope. By addressing workforce shortages, reducing administrative burdens, improving reimbursement models, and embracing technological advancements thoughtfully, we can begin to rebuild and strengthen our primary care system. The future of healthcare depends on it. It’s time for a collective effort – from policymakers to healthcare providers to patients – to ensure everyone has access to the quality primary care they deserve.
FAQ Resource
What are the most common reasons for physician burnout in primary care?
Long hours, excessive paperwork, emotional toll of patient care, and feeling undervalued are major contributors.
How does administrative burden affect patient care?
It reduces the time physicians can spend with patients, leading to rushed appointments and potentially missed diagnoses or preventative measures.
What are some innovative models of primary care delivery?
Team-based care, concierge medicine, and the use of health coaches are examples of innovative models aiming to improve efficiency and patient outcomes.
Can telehealth fully replace in-person primary care?
While telehealth offers advantages, it’s not a complete replacement. In-person visits remain crucial for certain examinations and patient-physician relationships.