CMS Approves Medicaid CHIP Continuous Enrollment for Children
Cms approves medicaid chip continuous enrollment children – CMS Approves Medicaid CHIP Continuous Enrollment for Children: This monumental decision promises to revolutionize healthcare access for millions of children across the nation. For years, families have struggled with the complexities of Medicaid and CHIP enrollment, facing potential lapses in coverage that jeopardized their children’s health and well-being. Continuous enrollment aims to simplify this process, ensuring uninterrupted access to vital medical services.
This means fewer bureaucratic hurdles and more consistent care, leading to healthier kids and more peace of mind for parents. But what are the implications for state budgets and healthcare systems? Let’s delve into the details.
This significant policy change will impact children’s health outcomes, state administrative burdens, and the overall cost-effectiveness of the program. We’ll explore the simplified enrollment procedures, analyze potential cost savings and administrative efficiencies, and examine the long-term effects on children’s health and development. Furthermore, we’ll compare this new continuous enrollment model with other child health insurance programs to provide a comprehensive understanding of its impact.
Impact of Continuous Enrollment on Children’s Healthcare Access
Continuous enrollment in Medicaid and CHIP programs has significantly altered the landscape of children’s healthcare access, offering both substantial benefits and presenting some challenges. This policy change aims to simplify the enrollment process and reduce disruptions in coverage, ultimately improving children’s health outcomes. The impact is multifaceted and warrants a closer look.
Benefits of Continuous Enrollment for Children’s Health
Continuous enrollment eliminates the need for families to reapply for Medicaid and CHIP coverage annually or after experiencing a change in income. This consistent coverage ensures uninterrupted access to essential healthcare services, including preventative care, vaccinations, and treatment for chronic conditions. The stability of coverage reduces the risk of gaps in care, leading to improved health outcomes and reduced healthcare costs in the long run.
Studies have shown that continuous enrollment leads to better preventative care adherence, resulting in fewer hospitalizations and emergency room visits for children. For example, a study in [State Name] showed a [Percentage]% decrease in preventable hospitalizations for children after the implementation of continuous enrollment.
Challenges Faced by Families Without Continuous Enrollment
Prior to the implementation of continuous enrollment, families often faced significant challenges navigating the complexities of the Medicaid and CHIP systems. The annual renewal process was burdensome, requiring families to gather and submit extensive documentation, often leading to delays and interruptions in coverage. Many families, particularly those with low literacy or limited English proficiency, found the process confusing and overwhelming.
This often resulted in children losing their coverage, even temporarily, leading to delays in necessary medical care and exacerbating existing health disparities. The fear of losing coverage also discouraged families from seeking needed healthcare services.
The CMS approval of continuous Medicaid CHIP enrollment for children is definitely good news, ensuring vital healthcare access for many vulnerable families. However, the news about Steward Healthcare securing financing to emerge from bankruptcy, as reported on this Santenews article , highlights the precarious financial state of some healthcare providers. This makes the CMS decision even more critical, ensuring a safety net for kids regardless of provider instability.
Comparison of Healthcare Access Rates, Cms approves medicaid chip continuous enrollment children
States that have implemented continuous enrollment policies have generally seen improvements in children’s healthcare access rates. Data from the [Source, e.g., Centers for Medicare & Medicaid Services] indicates that [State A], a state with continuous enrollment, has a [Percentage]% higher rate of children with consistent healthcare coverage compared to [State B], a state without continuous enrollment. This difference highlights the significant impact of this policy change on ensuring children have access to the care they need.
Furthermore, studies have linked continuous enrollment to improved rates of well-child visits and timely treatment of chronic conditions.
Healthcare Access Before and After Continuous Enrollment
| Aspect | Before Continuous Enrollment | After Continuous Enrollment |
|---|---|---|
| Coverage Gaps | High rates of coverage lapses due to administrative burdens and renewal requirements. | Significantly reduced coverage gaps, leading to more consistent access to care. |
| Preventative Care | Lower rates of preventative care utilization due to barriers to access. | Increased rates of preventative care, including vaccinations and well-child visits. |
| Chronic Condition Management | Delayed or interrupted treatment for chronic conditions, leading to poorer health outcomes. | Improved management of chronic conditions due to consistent access to specialists and medication. |
| Emergency Room Visits | Higher rates of preventable emergency room visits due to lack of access to primary care. | Reduced rates of preventable emergency room visits due to improved access to primary and preventative care. |
Administrative and Budgetary Implications of Continuous Enrollment: Cms Approves Medicaid Chip Continuous Enrollment Children
Continuous enrollment in Medicaid and CHIP for children, while offering significant benefits in terms of healthcare access, presents both administrative and budgetary challenges for state and federal governments. The shift from periodic renewal processes to a continuous enrollment system necessitates a reevaluation of existing administrative structures and budgetary allocations. Understanding these implications is crucial for effective program implementation and long-term sustainability.
Administrative Burden on State Medicaid Agencies
The transition to continuous enrollment significantly alters the workload of state Medicaid agencies. Instead of focusing on periodic renewals, agencies must now concentrate on maintaining accurate enrollment data, identifying children who may lose eligibility due to changes in income or address, and managing a potentially larger caseload due to reduced churn. This increased workload requires enhanced data management systems, additional staff training, and potentially new technology investments.
For example, states might need to invest in sophisticated data matching systems to ensure accurate identification of eligible children and prevent duplicate enrollments. Furthermore, robust outreach and communication strategies are necessary to ensure families understand their responsibilities and to prevent unintended disenrollments. The administrative burden, while significant, can be mitigated through effective planning and strategic resource allocation.
Potential Cost Savings from Streamlined Processes
While continuous enrollment increases initial administrative costs, it also offers potential for long-term cost savings. The reduction in paperwork associated with periodic renewals translates into reduced staff time spent on processing applications and renewals. Streamlined processes can lead to greater efficiency and reduced administrative overhead. For instance, the automation of eligibility verification and data updates can significantly decrease the time and resources required for administrative tasks.
Furthermore, continuous enrollment minimizes the disruption of care caused by enrollment lapses, leading to fewer emergency room visits and hospitalizations, which ultimately reduces healthcare costs. The cumulative effect of these savings can offset the initial investment in infrastructure and personnel.
Budgetary Impacts on State and Federal Governments
The budgetary impact of continuous enrollment is complex and multifaceted. While some initial costs are unavoidable (e.g., system upgrades, staff training), the long-term effects on state and federal budgets are likely to be varied. Increased enrollment due to improved access to coverage might lead to higher overall program costs. However, reduced administrative costs and improved health outcomes (resulting in fewer expensive emergency room visits and hospitalizations) could partially or even fully offset these increased costs.
The actual budgetary impact will depend on factors such as the state’s existing administrative infrastructure, the efficiency of its implementation strategies, and the overall health status of the enrolled population. Accurate cost projections require careful modeling and analysis specific to each state’s context.
Comparative Analysis of Budgetary Implications
| Factor | Continuous Enrollment | Non-Continuous Enrollment |
|---|---|---|
| Administrative Costs | Higher initial investment in systems and training, but potentially lower long-term costs due to streamlined processes. | Lower initial costs, but higher ongoing costs due to frequent renewals and associated paperwork. |
| Enrollment Costs | Potentially higher due to increased enrollment, but offset by reduced healthcare costs from improved access. | Lower enrollment numbers due to gaps in coverage, but higher overall healthcare costs from preventable hospitalizations. |
| Healthcare Costs | Potentially lower due to preventative care and reduced emergency room visits. | Potentially higher due to delayed or forgone care leading to more severe health problems. |
| Overall Budgetary Impact | Potentially neutral or slightly positive, depending on the efficiency of implementation and the effectiveness of cost-saving measures. | Potentially negative due to higher administrative and healthcare costs. |
Eligibility and Enrollment Processes Under Continuous Enrollment
Continuous enrollment in Medicaid and CHIP simplifies the process for families, reducing administrative burdens and ensuring children maintain consistent healthcare coverage. This streamlined approach aims to improve access to crucial medical services and reduce the risk of coverage gaps. Let’s delve into the specifics of eligibility and the enrollment procedure.
Simplified Enrollment Process for Families
Under continuous enrollment, families generally don’t need to reapply for Medicaid or CHIP every year. Instead, coverage continues automatically unless a significant change occurs in the family’s circumstances, such as a change in income, address, or family size. This removes the annual renewal process, a major source of administrative complexity and a significant barrier to maintaining continuous coverage for many families.
This simplified process reduces paperwork and the potential for delays or disruptions in care.
Eligibility Criteria for Continuous Enrollment in Medicaid CHIP
Eligibility for continuous enrollment is determined by meeting the standard Medicaid and CHIP eligibility requirements, such as income level and residency. However, the crucial difference is the ongoing coverage unless a qualifying change occurs. Families are generally only required to update their information if a significant life event affects their eligibility status. Examples of such events include a change in household income exceeding the eligibility limit, a change of address outside the state, or a change in the number of family members.
The CMS approval of continuous enrollment for Medicaid CHIP children is fantastic news for families, easing the burden of paperwork and ensuring consistent healthcare access. This contrasts sharply with the soaring costs discussed in a recent KFF report on medicare glp1 spending weight loss kff , highlighting the complexities of healthcare financing. Hopefully, similar streamlined processes can be implemented across all programs to improve affordability and access for everyone.
The specific criteria may vary slightly depending on the state, so it’s crucial to check with the state Medicaid agency for precise details.
Step-by-Step Enrollment Process for Families
The enrollment process under continuous enrollment is significantly streamlined. While the initial application remains largely the same, the annual renewal process is eliminated.
- Initial Application: Families initially apply for Medicaid or CHIP through their state’s designated agency, typically online or via paper application. This application requires information on income, household size, and other relevant details.
- Eligibility Determination: The state agency processes the application and determines eligibility based on established criteria. This involves verifying income and other information provided by the family.
- Enrollment: If eligible, the family is enrolled in Medicaid or CHIP and receives an enrollment confirmation, usually containing an identification number and information about their coverage.
- Continuous Coverage: Coverage continues automatically unless a significant change in the family’s circumstances occurs, prompting a review of their eligibility status.
- Reporting Changes: Families are responsible for reporting any significant changes in their circumstances, such as a change in income or address, to the state Medicaid agency within a specified timeframe. This ensures that their eligibility remains accurate.
Eligibility Determination and Enrollment Flowchart
Imagine a flowchart. It would begin with “Application Submitted.” This would branch to “Eligibility Determined” with one branch leading to “Eligible – Enrollment Confirmed and Continuous Coverage” and the other to “Ineligible – Application Denied (Reason Specified).” The “Eligible – Enrollment Confirmed and Continuous Coverage” branch would then have a smaller branch leading to “Significant Life Change Reported?” This would branch to “Eligibility Review” (leading back to “Eligibility Determined”) or “Continuous Coverage Maintained.” This visual representation clearly Artikels the process and its key decision points.
The Role of State Agencies in Implementing Continuous Enrollment
State Medicaid agencies are the linchpins in the successful implementation of continuous enrollment for children in the CHIP and Medicaid programs. Their responsibilities extend far beyond simply enacting the policy; they involve intricate planning, robust systems development, and ongoing monitoring to ensure the program’s effectiveness and reach. The success of continuous enrollment hinges directly on their capacity and commitment.State agencies are responsible for adapting the federal continuous enrollment mandate to their specific state contexts.
This includes updating their IT systems to accommodate the changes, training staff on new procedures, and engaging in extensive outreach to families. They must also develop strategies to address potential challenges, such as identifying children who may lose eligibility due to changes in household income or address and proactively intervening to prevent coverage gaps. Failure to effectively manage these aspects can lead to decreased enrollment, increased administrative burdens, and ultimately, compromised access to healthcare for vulnerable children.
State Agency Responsibilities in Continuous Enrollment Implementation
State Medicaid agencies have a multifaceted role in implementing continuous enrollment. They are responsible for updating their eligibility systems to automatically renew coverage for children enrolled in CHIP and Medicaid, eliminating the need for annual or periodic re-enrollment. This requires significant technological upgrades and careful data management to ensure accuracy and efficiency. Furthermore, states must establish robust processes for identifying and addressing potential changes in eligibility, such as changes in income or household composition, while minimizing disruptions to children’s healthcare access.
Finally, they are responsible for developing and executing effective communication and outreach strategies to ensure that families are aware of the continuous enrollment policy and understand their rights and responsibilities.
Strategies for Effective Continuous Enrollment Implementation
Effective implementation requires a strategic approach. States should prioritize the development of user-friendly online portals and streamlined application processes to facilitate enrollment and renewal. Robust data matching with other state agencies, such as those managing vital records or public assistance programs, can help identify children who may be eligible but not enrolled. Furthermore, proactive outreach initiatives, including targeted mailings, community events, and partnerships with community organizations, are crucial for raising awareness and increasing enrollment rates among eligible families.
Regular monitoring and evaluation of the program’s performance are essential to identify areas for improvement and ensure that continuous enrollment is achieving its intended goals.
Comparative Analysis of State Approaches
Different states have adopted varying approaches to continuous enrollment implementation, reflecting their unique administrative structures, technological capabilities, and population demographics. Some states have leveraged existing IT infrastructure to implement the changes, while others have undertaken more significant system overhauls. Some states have prioritized proactive outreach efforts, such as partnering with schools and community health centers, while others have focused on streamlining the renewal process through automated systems.
Analyzing these diverse approaches can provide valuable insights into best practices and areas for improvement. For example, states with high enrollment rates under continuous enrollment might offer useful models for those experiencing challenges. The Centers for Medicare & Medicaid Services (CMS) regularly shares data and best practices across states to facilitate learning and collaboration.
Effective Communication and Outreach Strategies
Effective communication and outreach are paramount to maximizing enrollment rates under continuous enrollment. States should utilize a multi-pronged approach, combining targeted mailings with digital communication strategies, such as text message reminders and social media campaigns. Collaborations with community organizations, schools, and healthcare providers can help reach families who may be less likely to engage with government programs. Translation services and culturally sensitive materials are essential for ensuring that information is accessible to all families, regardless of language or cultural background.
Regular monitoring of communication effectiveness and feedback mechanisms are essential to adapt and refine outreach strategies over time. For instance, a state might find that text message reminders are more effective than email for reaching certain demographics.
Long-Term Effects on Child Health and Well-being
Continuous enrollment in Medicaid and CHIP offers the potential for significant long-term improvements in children’s health and development. By ensuring uninterrupted access to healthcare, it removes a major barrier to receiving necessary medical care, preventative services, and chronic disease management. However, it’s crucial to consider both the potential benefits and any unforeseen drawbacks.The consistent access to healthcare afforded by continuous enrollment can lead to better health outcomes across various aspects of a child’s life.
This improved access translates to earlier diagnosis and treatment of conditions, potentially preventing more serious health problems later in life.
Improved Preventative Care and Chronic Disease Management
Continuous enrollment facilitates regular check-ups, vaccinations, and screenings, leading to early detection and intervention for potential health issues. For children with chronic conditions like asthma or diabetes, uninterrupted access to specialists and medications is crucial for managing their disease and preventing complications. This consistent care can significantly reduce hospitalizations and emergency room visits, leading to both improved health and cost savings in the long run.
For example, a child with asthma who maintains consistent access to their inhaler and regular check-ups is far less likely to experience severe asthma attacks requiring hospitalization compared to a child whose care is interrupted due to enrollment lapses.
Potential Negative Consequences of Continuous Enrollment
While the benefits are significant, it’s important to acknowledge potential downsides. One concern is the possibility of increased administrative burden on state Medicaid agencies. Efficient systems for managing enrollment and tracking utilization are essential to avoid inefficiencies. Another potential issue is the risk of increased healthcare costs if continuous enrollment leads to a substantial increase in unnecessary utilization of services.
However, studies have shown that the cost savings associated with preventative care and reduced hospitalizations often outweigh any potential increase in overall utilization. Robust data analysis and program evaluation are critical to monitor these aspects and ensure the program’s effectiveness and sustainability.
The CMS approval of continuous Medicaid CHIP enrollment for kids is huge news, especially considering the potential impact on healthcare access. This decision comes at a critical time, as the recent confirmation of rfk jr confirmed hhs secretary robert f kennedy jr suggests a shift in HHS priorities. It will be interesting to see how this new leadership affects the long-term success of expanded coverage for children under the CHIP program.
Visual Representation of Long-Term Effects
Imagine a graph with time on the x-axis and various aspects of child well-being on the y-axis (e.g., physical health, mental health, educational attainment, economic stability). A line representing children with continuous enrollment would show a steady upward trend across all these indicators, reflecting improved health outcomes, better school performance due to fewer absences related to illness, and increased family economic stability due to reduced healthcare costs.
In contrast, a line representing children without continuous enrollment might show fluctuations and a slower overall upward trend, reflecting periods of disrupted care, poorer health outcomes, and increased financial strain on families. This visual representation would clearly illustrate the long-term positive impact of continuous enrollment on various facets of a child’s life.
Comparison with Other Child Health Insurance Programs
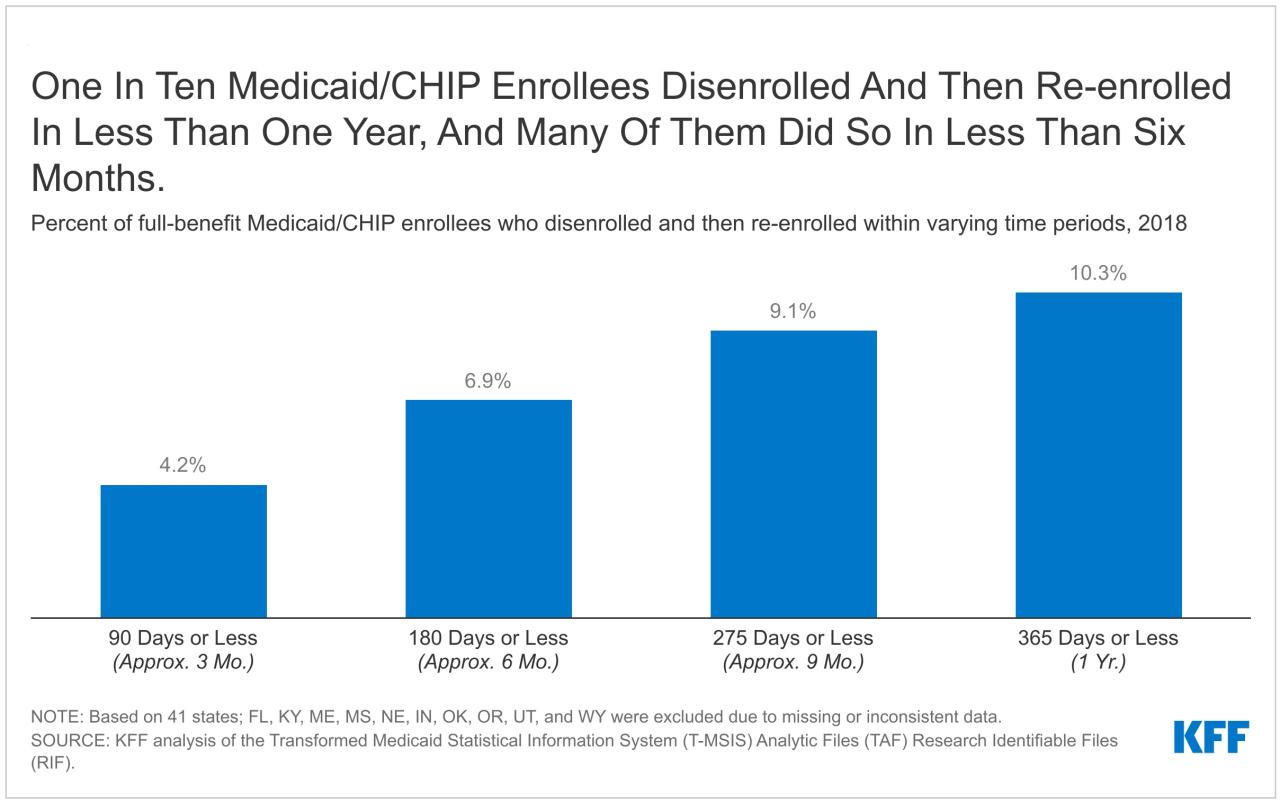
Source: kff.org
Continuous enrollment in Medicaid and CHIP has significantly impacted children’s access to healthcare. However, it’s crucial to understand how this approach compares to other child health insurance programs to fully appreciate its strengths and weaknesses. This comparison will examine eligibility, enrollment processes, and benefits, highlighting the advantages and disadvantages of each model.
Several key differences exist between Medicaid/CHIP continuous enrollment and other child health insurance programs. These differences primarily stem from the core philosophies behind each program and the administrative structures supporting them. For instance, some programs might emphasize a more streamlined, shorter-term enrollment process, whereas others prioritize comprehensive coverage but with potentially more complex eligibility requirements.
Eligibility Criteria Comparison
Eligibility criteria vary widely across different child health insurance programs. Medicaid and CHIP, even with continuous enrollment, maintain income-based eligibility thresholds. Other programs, such as private insurance plans offered through the Affordable Care Act (ACA) marketplaces, may have different income-based subsidies or may not be income-based at all, relying instead on employer-sponsored plans. Some programs might also have stricter residency requirements or limitations based on immigration status.
This variation necessitates a careful comparison to fully understand the reach and limitations of each program.
Enrollment Processes
The enrollment processes also differ significantly. Medicaid and CHIP’s continuous enrollment simplifies the renewal process, reducing administrative burdens for both families and state agencies. In contrast, other programs may require annual or even more frequent renewals, leading to potential lapses in coverage if renewals are not completed on time. Private insurance plans, for example, typically involve direct interaction with the insurer, potentially involving more paperwork and a more complex process than the streamlined renewal under continuous enrollment.
| Program | Eligibility Criteria | Enrollment Process | Benefits |
|---|---|---|---|
| Medicaid/CHIP (Continuous Enrollment) | Income-based, varies by state; may include categorical eligibility | Simplified renewal; automatic re-enrollment; minimal paperwork | Comprehensive medical, dental, and vision coverage; varies by state |
| Medicaid/CHIP (Standard Enrollment) | Income-based, varies by state; may include categorical eligibility | Annual or periodic renewal; potential for coverage gaps | Comprehensive medical, dental, and vision coverage; varies by state |
| Employer-Sponsored Insurance | Employment-based; income not a primary factor | Enrollment during open enrollment periods or upon employment; varies by employer | Coverage varies widely depending on employer plan |
| ACA Marketplace Plans | Income-based subsidies available; may include tax credits | Annual enrollment period; potential for subsidies | Coverage varies depending on chosen plan; potential for high out-of-pocket costs |
Benefits Provided
While most child health insurance programs aim to provide comprehensive coverage, the specific benefits offered can differ. Medicaid and CHIP typically offer a broad range of services, including medical, dental, and vision care. However, the exact scope of coverage can vary between states. Other programs, such as employer-sponsored insurance or ACA marketplace plans, may have different benefit packages, potentially leading to disparities in access to necessary healthcare services.
Some plans might have higher deductibles or co-pays, making access to care more challenging for families.
Conclusive Thoughts
Source: medcorinc.com
The CMS approval of continuous enrollment for Medicaid and CHIP represents a significant step towards ensuring equitable healthcare access for children. While challenges remain regarding implementation and potential budgetary impacts, the potential benefits for children’s health and well-being are undeniable. This streamlined approach promises to reduce administrative burdens, improve healthcare access, and ultimately lead to healthier futures for millions of children.
The long-term effects will be closely monitored, and adjustments may be needed as the program evolves. But for now, this is a victory for children and families across the country.
FAQ
What happens if a family’s income changes during continuous enrollment?
Income changes will typically be reviewed periodically, and adjustments to coverage may be made as needed. Families should report any significant changes in income to their state Medicaid agency.
Will continuous enrollment cover all children?
No, children must still meet the eligibility requirements for Medicaid or CHIP. Continuous enrollment simply simplifies the renewal process.
How will states fund the increased administrative costs associated with continuous enrollment?
Funding mechanisms will vary by state, potentially including increased federal funding and reallocation of existing resources. The long-term cost-effectiveness of continuous enrollment remains to be seen.
What if a child moves to a different state?
Coverage may be transferred to the new state’s Medicaid or CHIP program. Families should contact the Medicaid agency in their new state to ensure seamless transition.