HHS Voluntary Healthcare Cybersecurity Goals
HHS Voluntary Healthcare Cybersecurity Goals: Protecting patient data in the digital age is a monumental task, and the HHS’s voluntary cybersecurity goals are a crucial step towards a safer healthcare landscape. This initiative aims to bolster cybersecurity practices across the healthcare industry, tackling the ever-growing threat of data breaches and cyberattacks. Let’s dive into what these goals entail, how they’re implemented, and the challenges faced along the way.
The initiative isn’t just about compliance; it’s about fostering a culture of proactive security. By encouraging voluntary adoption, the HHS hopes to empower healthcare organizations to build robust defenses, ultimately safeguarding sensitive patient information and maintaining public trust. This isn’t just about checking boxes; it’s about building a stronger, more resilient healthcare system capable of withstanding the evolving threats of the digital world.
HHS Voluntary Healthcare Cybersecurity Goals
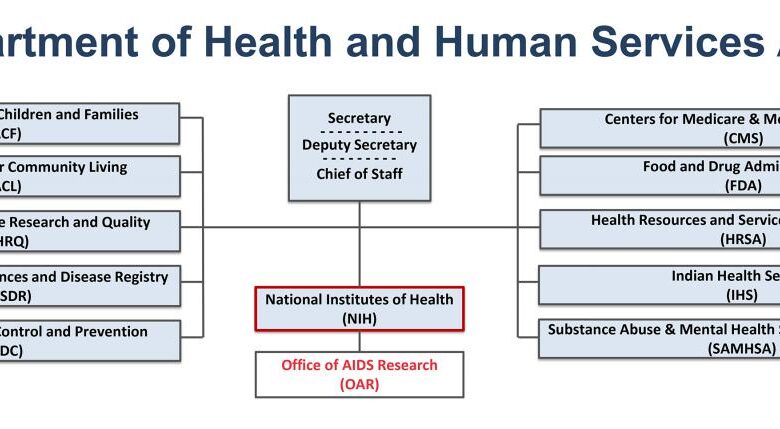
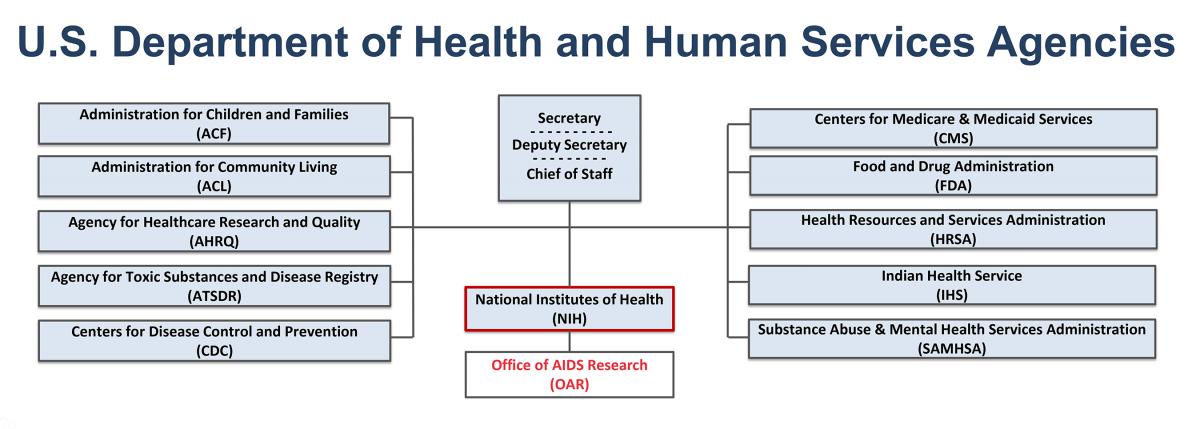
The Department of Health and Human Services (HHS) has established voluntary cybersecurity goals for healthcare organizations to enhance the security of protected health information (PHI) and bolster the overall resilience of the healthcare sector against cyber threats. These goals aren’t legally mandated but serve as a framework for best practices and encourage proactive cybersecurity measures. Adoption demonstrates a commitment to patient data protection and operational integrity.The key objectives of the HHS voluntary cybersecurity goals are to improve the overall cybersecurity posture of healthcare providers and their associated entities.
The HHS voluntary healthcare cybersecurity goals are crucial for protecting patient data, especially as we grapple with increasing digitalization. A significant challenge is the strain on healthcare systems, exacerbated by the medical coding worker shortage; addressing this requires innovative solutions, like those discussed in the ai powered solution to the medical coding worker shortage. Ultimately, improved efficiency through AI can free up resources to bolster cybersecurity efforts, aligning perfectly with the HHS goals.
This involves strengthening defenses against a range of cyber threats, including ransomware attacks, phishing scams, and data breaches. The initiative aims to standardize cybersecurity practices, promote information sharing, and encourage the adoption of robust risk management strategies. It’s a collaborative effort to foster a more secure healthcare ecosystem.These goals are intended to have a significant positive impact on healthcare organizations.
By implementing the recommended practices, organizations can reduce their vulnerability to cyberattacks, minimize the risk of data breaches, and protect the confidentiality, integrity, and availability of patient data. Improved cybersecurity also leads to enhanced operational efficiency, reduced financial losses associated with breaches, and increased patient trust and confidence. Furthermore, it strengthens compliance with existing regulations such as HIPAA.Examples of Healthcare Organizations that Have Adopted these Goals are not publicly listed in a comprehensive, centralized manner by HHS.
The voluntary nature of the initiative means organizations aren’t required to publicize their adoption. However, many large healthcare systems and hospitals actively participate in cybersecurity initiatives aligned with the HHS goals. This often involves participation in information sharing and analysis centers (ISACs), adoption of industry-recognized cybersecurity frameworks (like NIST Cybersecurity Framework), and investment in advanced security technologies.
The emphasis is on proactive risk management, rather than solely reactive responses to breaches.
Key Objectives of the HHS Voluntary Cybersecurity Goals
The HHS voluntary cybersecurity goals focus on several key areas to improve the security of healthcare data and systems. These areas include establishing a robust cybersecurity program, implementing strong access controls, regularly backing up data, and maintaining up-to-date software and systems. A comprehensive approach is vital for effective protection.
Impact on Healthcare Organizations
Adoption of these goals leads to a multitude of benefits for healthcare organizations. Reduced risk of data breaches, improved patient trust, enhanced operational efficiency, and better compliance with regulations are key advantages. These improvements translate to cost savings and enhanced reputation.
Key Components of the HHS Cybersecurity Framework
The HHS Cybersecurity Framework isn’t a rigid set of regulations, but rather a flexible guide designed to help healthcare organizations manage and reduce cybersecurity risks. It emphasizes a risk-based approach, allowing organizations to tailor their security practices to their specific size, resources, and the unique threats they face. This adaptability is crucial given the diverse landscape of the healthcare sector, ranging from small clinics to large hospital systems.The framework’s core is built around five key functions: Identify, Protect, Detect, Respond, and Recover.
These functions are interconnected and iterative, meaning organizations continuously cycle through them, adapting their strategies as threats evolve. This cyclical approach reflects the dynamic nature of cybersecurity, where constant vigilance and adaptation are paramount.
Risk Management within the HHS Cybersecurity Framework
Risk management is the cornerstone of the HHS Cybersecurity Framework. It’s not just about identifying vulnerabilities; it’s about understanding the likelihood and potential impact of those vulnerabilities turning into actual incidents. This involves a thorough assessment of assets, threats, and vulnerabilities, followed by a prioritization of risks based on their potential damage. For example, a hospital might prioritize protecting patient data more highly than protecting less sensitive administrative data, reflecting the greater potential harm from a data breach affecting patient records.
The framework encourages organizations to use a variety of risk management methodologies and tools, tailoring their approach to their specific context. This might involve quantitative risk assessments using statistical models or qualitative assessments based on expert judgment. The output informs resource allocation and the development of mitigation strategies.
Data Security and Privacy in the HHS Cybersecurity Framework
Data security and privacy are inextricably linked to the overall success of the framework. The framework emphasizes the importance of protecting patient data, adhering to regulations like HIPAA, and implementing robust data security controls. This includes measures like encryption, access controls, and data loss prevention (DLP) tools. Furthermore, the framework encourages organizations to develop comprehensive data governance policies that define data ownership, access rights, and data retention policies.
Failing to adequately protect patient data not only exposes organizations to significant financial and reputational damage but also poses a serious risk to patient safety and well-being. A breach could lead to identity theft, medical errors, and erosion of patient trust.
Comparison with Other Cybersecurity Frameworks
The HHS Cybersecurity Framework shares similarities with other frameworks, such as the NIST Cybersecurity Framework, but also has unique aspects reflecting the specific needs of the healthcare industry. While NIST provides a broader, industry-agnostic approach, the HHS framework incorporates specific regulatory requirements and considerations relevant to healthcare, such as HIPAA compliance. Both frameworks, however, emphasize a risk-based approach and the importance of continuous improvement.
Other frameworks, like the CIS Controls, may offer a more prescriptive set of security controls, whereas the HHS framework provides a more flexible guidance. The key difference lies in the tailored focus; HHS prioritizes the unique challenges and vulnerabilities present within the healthcare sector, aligning with its regulatory landscape and the sensitivity of patient data.
Implementation Strategies and Best Practices
Successfully implementing the HHS cybersecurity goals requires a phased approach, integrating cybersecurity into the existing healthcare workflow without disrupting patient care. This involves careful planning, resource allocation, and a commitment to continuous improvement. The following sections Artikel a practical implementation plan and best practices for achieving and maintaining compliance.
Step-by-Step Implementation Plan for Adopting HHS Cybersecurity Goals
A structured approach is crucial for effective implementation. This plan breaks down the process into manageable steps, allowing for continuous assessment and adjustment.
- Assessment and Prioritization: Begin with a thorough risk assessment identifying vulnerabilities and prioritizing systems based on criticality (e.g., EHR systems, patient data repositories). This assessment should include a review of existing security controls and their effectiveness.
- Policy Development and Training: Develop and implement comprehensive cybersecurity policies, procedures, and training programs for all staff. These should address data access, password management, incident response, and phishing awareness. Regular training refreshers are vital.
- Technology Implementation: Implement necessary technologies to address identified vulnerabilities. This might include firewalls, intrusion detection systems, endpoint protection, data loss prevention tools, and multi-factor authentication. Prioritize solutions based on the risk assessment.
- Vulnerability Management: Establish a robust vulnerability management program that includes regular vulnerability scanning, penetration testing, and timely patching of identified vulnerabilities. This is an ongoing process requiring continuous monitoring and updates.
- Incident Response Planning: Develop and test a comprehensive incident response plan that Artikels procedures for handling security incidents, including data breaches. This plan should include communication protocols and a process for reporting incidents to relevant authorities.
- Monitoring and Auditing: Implement continuous security monitoring to detect and respond to threats in real-time. Regular security audits are essential to verify the effectiveness of implemented controls and ensure ongoing compliance.
- Continuous Improvement: Cybersecurity is an ongoing process. Regularly review and update policies, procedures, and technologies to adapt to evolving threats and best practices. This requires a culture of continuous learning and improvement.
Best Practices for Achieving Cybersecurity Compliance
Achieving and maintaining cybersecurity compliance demands a multifaceted approach that extends beyond technology.
- Strong Password Policies: Enforce strong, unique passwords and encourage the use of password managers.
- Multi-Factor Authentication (MFA): Implement MFA for all critical systems and user accounts to enhance security.
- Regular Security Awareness Training: Conduct regular training sessions to educate staff on cybersecurity threats and best practices. Simulate phishing attacks to test employee awareness.
- Data Encryption: Encrypt sensitive data both in transit and at rest to protect against unauthorized access.
- Access Control: Implement robust access control measures, granting only necessary access to data and systems based on the principle of least privilege.
- Regular Security Audits and Penetration Testing: Conduct regular security audits and penetration testing to identify vulnerabilities and assess the effectiveness of security controls.
- Incident Response Plan: Develop and regularly test a comprehensive incident response plan to effectively handle security incidents.
- Vendor Risk Management: Assess the security posture of third-party vendors and ensure they meet your organization’s security requirements.
Integrating Cybersecurity into Existing Healthcare Workflows, Hhs voluntary healthcare cybersecurity goals
Seamless integration is key to avoiding disruptions. This requires careful consideration of workflow optimization and staff training.Cybersecurity should not be a separate function but an integral part of daily operations. For example, integrating security checks into existing processes, such as patient admission or medication dispensing, ensures that security practices are followed consistently. Workflow redesign might be necessary in some cases to incorporate new security measures without hindering efficiency.
Training staff on new security protocols and integrating security considerations into all aspects of the workflow are vital for success. This requires clear communication and a collaborative approach across departments.
Comparison of Implementation Approaches
| Approach | Cost | Time to Implement | Effectiveness |
|---|---|---|---|
| Phased Approach (Prioritized Risk Mitigation) | Moderate to High (depending on scope) | 6-12 months or more | High (allows for iterative improvements) |
| Big Bang Approach (Complete Overhaul) | High | Short to Medium (potential for significant disruption) | Potentially High (but risks are significant) |
| Outsourcing to a Managed Security Service Provider (MSSP) | Moderate to High (depending on services) | Short to Medium (depending on scope) | Moderate to High (dependent on MSSP capabilities) |
| Hybrid Approach (Combining Internal Resources with External Support) | Moderate | Medium | High (balances cost and expertise) |
Challenges and Barriers to Adoption
The HHS voluntary cybersecurity goals, while laudable, face significant hurdles in their widespread adoption across the healthcare sector. These challenges stem from a complex interplay of resource limitations, expertise gaps, and the inherent complexities of the healthcare IT landscape. Successfully navigating these obstacles requires a multi-faceted approach that addresses both the technical and organizational aspects of cybersecurity implementation.
Resource Constraints
Healthcare organizations, particularly smaller clinics and rural hospitals, often grapple with limited financial and personnel resources. Implementing robust cybersecurity measures requires substantial investments in hardware, software, training, and ongoing maintenance. The cost of advanced security technologies, like intrusion detection systems and security information and event management (SIEM) tools, can be prohibitive for organizations with already tight budgets. This financial strain can lead to a prioritization of other pressing needs, often leaving cybersecurity initiatives underfunded and understaffed.
For example, a small rural hospital might prioritize purchasing new medical equipment over investing in a comprehensive cybersecurity program, even though a breach could have far more devastating long-term consequences.
The HHS voluntary healthcare cybersecurity goals aim to strengthen data protection across the board, impacting everything from patient records to research data. This is especially crucial when considering the sensitive information involved in managing conditions like Tourette Syndrome; for helpful guidance on this, check out this resource on strategies to manage Tourette syndrome in children. Ultimately, robust cybersecurity safeguards are vital to protecting all patient health information, regardless of the specific condition.
Limited Cybersecurity Expertise
A critical barrier to adoption is the shortage of qualified cybersecurity professionals. Many healthcare organizations lack the in-house expertise to effectively implement and manage complex cybersecurity programs. Finding and retaining skilled cybersecurity personnel is competitive, with higher salaries often offered in other sectors. This shortage results in a reliance on external consultants, which can be expensive and may not provide the same level of ongoing support and integration within the organization.
This lack of internal expertise also means that organizations may struggle to properly assess their vulnerabilities, respond effectively to incidents, and stay abreast of evolving threats. A hypothetical scenario: a hospital’s IT department might lack the skills to detect a sophisticated phishing attack, leading to a data breach with significant repercussions.
Overcoming Challenges
Addressing these challenges requires a multi-pronged strategy. Financial incentives, such as government grants or subsidies, could help alleviate the resource constraints faced by smaller organizations. Furthermore, collaborative efforts, including the sharing of best practices and resources among healthcare providers, can improve cybersecurity capabilities without requiring each organization to independently shoulder the entire burden. Investing in cybersecurity training programs and educational initiatives can help develop a more robust pipeline of skilled professionals within the healthcare sector.
Finally, the development of user-friendly and cost-effective cybersecurity tools tailored to the specific needs of healthcare organizations can significantly increase adoption rates. For example, simplified security awareness training programs, easily integrated into existing workflows, could dramatically improve employee vigilance against phishing attempts and other common threats.
Measuring Success and Assessing Effectiveness
Successfully implementing the HHS Voluntary Healthcare Cybersecurity Framework requires a robust system for measuring progress and evaluating the effectiveness of implemented security measures. This goes beyond simply checking boxes; it involves continuous monitoring, data-driven analysis, and a commitment to improvement based on real-world performance. Without a clear understanding of what constitutes success, organizations risk investing resources without achieving meaningful improvements in their cybersecurity posture.
The HHS voluntary healthcare cybersecurity goals aim to strengthen data protection across the board, impacting everything from patient records to research findings. This is especially crucial when considering how advancements in early detection methods, like those discussed in this fascinating article on whether can eye test detect dementia risk in older adults , could impact future healthcare data management and security protocols.
Ultimately, robust cybersecurity is vital for protecting sensitive health information, no matter the source or application.
Key Performance Indicators (KPIs) for Cybersecurity Progress
Tracking progress requires a set of measurable KPIs. These should align with the specific goals and objectives of the organization’s cybersecurity program, reflecting the framework’s core functions. Choosing the right KPIs is crucial, as they will drive decision-making and resource allocation. Poorly chosen KPIs can lead to misdirected efforts and a false sense of security.
- Mean Time To Detect (MTTD): This metric measures the average time it takes to identify a cybersecurity incident. A lower MTTD indicates a more effective detection system. For example, a target MTTD might be reduced from 72 hours to 24 hours within a year.
- Mean Time To Respond (MTTR): This measures the average time it takes to contain and remediate a security incident. A lower MTTR demonstrates improved incident response capabilities. A goal might be to reduce MTTR from 48 hours to 12 hours over a two-year period.
- Number of Successful Phishing Attacks: Tracking the number of successful phishing attempts highlights vulnerabilities in employee training and awareness programs. A significant reduction in this number indicates the effectiveness of security awareness training initiatives.
- Percentage of Systems with Up-to-Date Patches: This metric measures the organization’s adherence to patching schedules. A higher percentage indicates better protection against known vulnerabilities. A target might be to achieve 98% patch compliance within six months.
- Number of Security Incidents: While a reduction in the overall number of incidents is desirable, the focus should also be on the severity and impact of those incidents. A reduction in high-severity incidents is more meaningful than a reduction in low-severity incidents.
Cybersecurity Incident Tracking and Reporting
A standardized process for tracking and reporting cybersecurity incidents is critical for identifying trends, improving response times, and demonstrating compliance. This process should include detailed documentation of each incident, including its nature, impact, and remediation steps. Regular reporting to relevant stakeholders, such as senior management and regulatory bodies, is also essential.The system should include a centralized database to log all incidents, enabling efficient analysis and reporting.
Reports should be generated regularly, providing insights into incident trends and the effectiveness of security controls. For example, a monthly report summarizing all incidents, categorized by type and severity, would be beneficial. A quarterly report could analyze trends and identify areas needing improvement.
Evaluating the Effectiveness of Security Measures
Regular evaluation of implemented security measures is necessary to ensure their ongoing effectiveness. This involves a combination of technical assessments, penetration testing, vulnerability scans, and employee training evaluations. The results of these evaluations should be used to inform improvements to the organization’s overall cybersecurity posture.For instance, post-implementation reviews of security controls, such as firewalls or intrusion detection systems, should be conducted to assess their effectiveness in blocking or detecting threats.
Regular penetration testing can identify weaknesses that might be exploited by malicious actors. Vulnerability scans help to identify and prioritize software vulnerabilities requiring patching. Finally, periodic employee training assessments can gauge the effectiveness of security awareness training programs.
Examples of Successful Implementations and Measurable Outcomes
Several healthcare organizations have demonstrated success in improving their cybersecurity posture through the implementation of the HHS Cybersecurity Framework. For example, a large hospital system might report a 50% reduction in successful phishing attacks after implementing a comprehensive security awareness training program. Another organization might showcase a 25% reduction in MTTR after investing in advanced security information and event management (SIEM) technology.
These quantifiable results demonstrate the value of a proactive approach to cybersecurity and the importance of continuous monitoring and improvement.
Future Trends and Considerations: Hhs Voluntary Healthcare Cybersecurity Goals
The healthcare cybersecurity landscape is constantly evolving, presenting both new opportunities and significant challenges. Maintaining the effectiveness of the HHS cybersecurity framework requires a proactive approach that anticipates and adapts to emerging threats and technological advancements. Failure to do so could result in devastating breaches, compromising patient data and disrupting critical healthcare services.The increasing interconnectedness of healthcare systems, driven by telehealth, the Internet of Medical Things (IoMT), and cloud computing, expands the attack surface exponentially.
This interconnectedness, while offering significant benefits, creates vulnerabilities that malicious actors can exploit. Understanding and mitigating these risks is crucial for maintaining the integrity and confidentiality of patient information.
Emerging Threats and Vulnerabilities
The threat landscape is dynamic and sophisticated. Ransomware attacks, specifically targeting healthcare providers due to their reliance on readily available data and the critical nature of their services, remain a significant concern. We’ve seen numerous high-profile incidents where hospitals have been forced to shut down critical systems, delaying or preventing essential patient care. Furthermore, the rise of AI-powered attacks, capable of bypassing traditional security measures, represents a growing threat.
These attacks can be incredibly difficult to detect and respond to, necessitating a shift towards more proactive and adaptive security strategies. Phishing attacks, exploiting human error, remain prevalent, highlighting the importance of robust employee training and awareness programs.
Impact of New Technologies
The integration of artificial intelligence (AI) and machine learning (ML) offers significant potential for enhancing healthcare cybersecurity. AI-powered security tools can automate threat detection, analysis, and response, improving the speed and efficiency of incident handling. However, the same technologies can also be weaponized by attackers, necessitating a thorough understanding of both the opportunities and risks associated with AI in cybersecurity.
Similarly, the widespread adoption of cloud computing presents both benefits (scalability, cost-effectiveness) and challenges (data security, compliance). A well-defined cloud security strategy is essential to ensure the protection of sensitive patient data stored in the cloud. The increasing use of IoMT devices introduces new vulnerabilities, as these devices often lack robust security features and can be easily compromised.
A comprehensive security strategy must address the unique vulnerabilities presented by these interconnected devices.
Adapting the HHS Framework to Future Challenges
The HHS cybersecurity framework needs to be regularly reviewed and updated to remain effective in the face of evolving threats and technologies. This requires a collaborative effort involving healthcare providers, technology vendors, and government agencies. Investing in advanced security technologies, such as AI-powered threat detection systems and robust endpoint protection, is crucial. Furthermore, a strong focus on employee training and awareness is essential to mitigate the risk of human error, which remains a significant vulnerability.
Regular security audits and penetration testing can help identify and address weaknesses in security posture. Finally, fostering a culture of cybersecurity awareness within healthcare organizations is paramount. This includes establishing clear roles and responsibilities, implementing effective incident response plans, and promoting ongoing education and training. This proactive approach will enable healthcare organizations to better adapt to the evolving cybersecurity landscape and protect sensitive patient data.
Illustrative Case Studies
Source: alamy.com
Examining real-world examples of both successful and unsuccessful implementations of the HHS cybersecurity framework provides valuable insights for healthcare organizations. These case studies highlight the tangible benefits of proactive security measures and the devastating consequences of neglecting cybersecurity best practices.
Successful Implementation: Memorial Healthcare System
Memorial Healthcare System (MHS), a large Florida-based healthcare provider, significantly improved its cybersecurity posture by proactively implementing several key components of the HHS Cybersecurity Framework. Recognizing the increasing sophistication of cyber threats, MHS invested heavily in employee training, focusing on phishing awareness and secure coding practices. This initiative alone dramatically reduced the number of successful phishing attacks targeting staff.
Furthermore, they implemented robust multi-factor authentication across all systems, significantly limiting unauthorized access. Their investment in advanced threat detection systems, including intrusion detection and prevention systems (IDPS), allowed for early identification and mitigation of potential breaches. Regular security audits and penetration testing identified vulnerabilities before they could be exploited. The combination of these proactive measures resulted in a demonstrably lower incidence of security incidents and a significant reduction in the overall risk to patient data and the organization’s operational continuity.
The financial investment in these upgrades, while substantial, was far outweighed by the cost savings from avoiding a major breach and maintaining public trust.
Negative Consequences of Inadequate Cybersecurity: A Hypothetical Case Study Based on Real-World Trends
While specific details of many breaches are often kept confidential for legal and competitive reasons, a composite case study reflecting common patterns can illustrate the negative consequences. Imagine a small regional hospital, “County General,” lacking a comprehensive cybersecurity program. Their IT infrastructure was outdated, with many systems running legacy software lacking critical security patches. They relied on basic password protection and lacked multi-factor authentication.
Employees received minimal cybersecurity training. This vulnerable environment made them an easy target for a ransomware attack. Hackers exploited a known vulnerability in their outdated billing system, encrypting patient data and demanding a significant ransom. The hospital was forced to shut down non-essential services for several days, impacting patient care and causing significant operational disruption. The ransom was paid, but the incident resulted in substantial financial losses, reputational damage, regulatory fines (including HIPAA violations), and a loss of patient trust.
The cost of recovery, including forensic investigation, data restoration, and legal fees, far exceeded the initial investment required for a robust cybersecurity program. The impact extended beyond immediate financial costs, impacting patient care, staff morale, and the hospital’s long-term viability.
Final Conclusion
Source: nih.gov
The journey towards stronger healthcare cybersecurity isn’t a sprint, it’s a marathon. The HHS voluntary goals provide a roadmap, but successful implementation requires commitment, resources, and a proactive approach. While challenges exist, the potential rewards – enhanced patient safety, reduced financial losses, and increased public confidence – make the effort undeniably worthwhile. By embracing these goals and continually adapting to the ever-changing threat landscape, the healthcare industry can move towards a future where data breaches are the exception, not the rule.
Answers to Common Questions
What happens if a healthcare organization doesn’t adopt the HHS voluntary goals?
While adoption is voluntary, non-compliance could increase the organization’s vulnerability to cyberattacks and regulatory scrutiny. It might also impact their reputation and public trust.
Are there financial incentives for adopting the HHS goals?
While not directly stated as financial incentives, improved cybersecurity can lead to reduced costs associated with data breaches, legal fees, and reputational damage. Furthermore, some insurers may offer preferential rates to organizations demonstrating strong cybersecurity posture.
How often are the HHS cybersecurity goals updated?
The HHS regularly reviews and updates its cybersecurity guidance to reflect the evolving threat landscape and technological advancements. Staying informed about these updates is crucial for maintaining effective security practices.
Can smaller healthcare organizations realistically implement these goals?
Yes, while resource constraints may be a challenge, the HHS framework offers flexibility. Smaller organizations can prioritize key areas based on their risk profile and gradually implement measures over time. External resources and collaborations can also assist in bridging resource gaps.





