HHS Ransomware Settlements South Dakota Healthcare Crisis
Hhs ransomware settlements plastic surgery assciates south dakota bryan county ambulance – HHS ransomware settlements involving Plastic Surgery Associates, a South Dakota clinic, and Bryan County Ambulance, highlight a terrifying reality for rural healthcare. This incident isn’t just about dollars and cents; it’s about the vulnerability of small healthcare providers to cyberattacks and the devastating consequences for patients and the community. Imagine the ripple effect – a compromised medical practice impacting not just patients’ privacy but also emergency services.
This story delves into the financial strain on the HHS, the legal battles, and the urgent need for better cybersecurity in rural areas.
We’ll explore the specific vulnerabilities exploited in the attack on Plastic Surgery Associates, the types of data compromised (think patient records, financial information, even medical images!), and the legal repercussions for the clinic. We’ll also look at how the ransomware attack might have indirectly affected Bryan County Ambulance, causing potential disruptions to emergency services. The ethical implications of data breaches and the long-term effects on patient trust are also key considerations.
HHS Ransomware Settlements in Bryan County, South Dakota
Source: b-cdn.net
The recent ransomware attacks affecting healthcare providers in Bryan County, South Dakota, highlight a critical vulnerability within our nation’s healthcare system, particularly in rural areas. These incidents underscore the significant financial and operational challenges faced by smaller healthcare facilities when dealing with cyber threats, and the ripple effect these attacks have on the broader healthcare landscape. The settlements reached with the HHS reflect the substantial costs associated with recovering from such attacks, costs ultimately borne by taxpayers and potentially impacting the quality of care provided.The Impact of Ransomware Attacks on Rural Healthcare ProvidersRansomware attacks disproportionately impact rural healthcare providers like those in Bryan County due to limited resources, both financial and technological.
The HHS ransomware settlements involving South Dakota’s Bryan County Ambulance and plastic surgery associates got me thinking about healthcare consolidation. It’s crazy how vulnerable these systems are, especially considering the FTC is now suing to block the Novant Health and Community Health Systems hospital acquisition, as reported here: federal trade commission sues block novant health community health systems hospital acquisition.
This just highlights the bigger picture of healthcare security and the potential for even larger entities to become targets if mergers aren’t carefully scrutinized. The whole situation with the Bryan County Ambulance and those settlements is a microcosm of a much larger problem.
Smaller facilities often lack the robust cybersecurity infrastructure and dedicated IT staff possessed by larger urban hospitals. This makes them more susceptible to attacks and less equipped to handle the aftermath. A successful ransomware attack can cripple operations, leading to disruptions in patient care, delays in treatment, and loss of sensitive patient data. The financial burden of recovery, including paying the ransom (in some cases), hiring cybersecurity experts, and restoring systems, can be devastating for already financially strained rural hospitals, potentially forcing them to cut services or even close.
The resulting loss of access to essential healthcare services can have profound consequences for the community.
Financial Burden of Ransomware Settlements on the HHS Budget
The financial burden of ransomware settlements on the HHS budget is substantial and growing. Each settlement represents a significant expenditure of taxpayer dollars, diverting funds from other essential healthcare programs and initiatives. While the exact figures for settlements related to Bryan County may not be publicly available due to confidentiality agreements, the overall cost of ransomware attacks to the HHS is immense and continues to escalate.
This financial strain forces difficult choices regarding resource allocation, potentially impacting funding for preventative healthcare measures, public health programs, and other critical services. The cumulative effect of numerous settlements across the country strains the HHS budget and ultimately undermines the agency’s ability to effectively fulfill its mission.
Comparison of Ransomware Attacks Targeting Small vs. Large Healthcare Facilities
Small healthcare facilities, such as those prevalent in rural areas like Bryan County, are significantly more vulnerable to ransomware attacks than larger systems. This vulnerability stems from several factors, including limited IT resources, outdated software and hardware, and a lack of comprehensive cybersecurity training for staff. While larger healthcare systems are also targets, they typically possess more sophisticated cybersecurity defenses, incident response plans, and dedicated IT teams to mitigate the impact of an attack.
The severity of attacks can also differ; while a ransomware attack on a small facility might completely disrupt its operations, a large system might experience localized disruptions, though still incurring significant costs. The frequency of successful attacks is also higher for smaller facilities due to their inherent vulnerabilities.
Hypothetical Risk Mitigation Strategy for Bryan County Healthcare Providers
A comprehensive risk mitigation strategy for Bryan County healthcare providers should incorporate several key elements. This includes investing in robust cybersecurity infrastructure, such as firewalls, intrusion detection systems, and endpoint detection and response solutions. Regular software updates and patching are crucial to address known vulnerabilities. Employee cybersecurity training is paramount to educate staff on phishing scams, malware, and other social engineering tactics.
So, the news about HHS ransomware settlements affecting places like plastic surgery associates in South Dakota and even Bryan County ambulance services is pretty wild, right? It makes you wonder what kind of security measures are in place. Given all this, the recent news that rfk jr confirmed hhs secretary robert f kennedy jr is a huge development.
His approach to healthcare security could significantly impact how these future HHS ransomware issues are handled, potentially changing the landscape of these settlements.
Developing and regularly testing a comprehensive incident response plan is essential to minimize the impact of a successful attack. This plan should Artikel procedures for containing the attack, recovering data, and notifying relevant authorities. Finally, establishing strong data backup and recovery procedures, including offsite backups, is vital to ensure business continuity in the event of a ransomware attack.
Regular cybersecurity assessments and penetration testing can help identify and address vulnerabilities before they can be exploited. Furthermore, collaborating with other healthcare providers in the region to share best practices and threat intelligence can significantly enhance collective cybersecurity posture.
Plastic Surgery Associates and the Ransomware Incident
Source: medbill.net
The ransomware attack on Plastic Surgery Associates in South Dakota, while not as widely publicized as some larger incidents, highlights the vulnerability of even smaller healthcare providers to cybercrime. Understanding the specifics of this attack, the data compromised, and the resulting legal implications provides valuable insight into the broader challenges facing the healthcare industry in protecting sensitive patient information.
Potential Vulnerabilities Exploited, Hhs ransomware settlements plastic surgery assciates south dakota bryan county ambulance
The exact vulnerabilities exploited in the Plastic Surgery Associates ransomware attack are likely unknown publicly, as details of such incidents are often kept confidential for security and legal reasons. However, common attack vectors for healthcare providers include phishing emails targeting employees, exploiting weaknesses in outdated software, and leveraging vulnerabilities in remote access tools. Given the nature of the business, a likely scenario involves a phishing email containing a malicious attachment or link that allowed the ransomware to gain access to the network.
Another possibility is an unpatched software vulnerability on a server or workstation, providing an entry point for the attackers. Regardless of the specific method, the lack of robust cybersecurity measures, such as multi-factor authentication, regular software updates, and employee security training, likely contributed to the success of the attack.
Data Compromised and Potential Consequences
The type of data compromised in a ransomware attack on a plastic surgery practice is particularly sensitive. Patient records likely included protected health information (PHI) such as names, addresses, dates of birth, medical history, insurance information, and potentially even images from procedures. Financial data, including billing information and credit card details, would also be at risk. The consequences for patients are significant.
Identity theft, medical identity theft (fraudulent use of medical insurance), and financial losses are all potential outcomes. The breach of trust between patients and the practice can also lead to reputational damage and loss of future business.
Legal Ramifications for Plastic Surgery Associates
Following a ransomware attack, Plastic Surgery Associates faces several potential legal ramifications. Compliance with HIPAA (Health Insurance Portability and Accountability Act) is paramount. Failure to properly secure patient data and to notify affected individuals in a timely manner can result in significant fines and legal action. Depending on the extent of the data breach and the resulting harm to patients, lawsuits from individuals or class-action lawsuits are also possible.
Furthermore, the practice may face regulatory investigations and penalties from state and federal agencies. Insurance coverage and the ability to recover from the attack’s financial impact will also be significant factors in navigating the legal aftermath.
Types of Data and Corresponding Security Risks
| Data Type | Security Risk |
| Patient Records (PHI) | Identity theft, medical identity theft, HIPAA violations, reputational damage, legal liabilities |
| Financial Data (Billing, Credit Card Information) | Financial fraud, identity theft, legal liabilities, regulatory penalties |
| Employee Data (Payroll, Personal Information) | Identity theft, legal liabilities, reputational damage |
| Operational Data (Business Records, Patient Scheduling) | Disruption of services, financial losses, reputational damage |
The Role of Bryan County Ambulance in the Incident
The ransomware attack on Plastic Surgery Associates (PSA) in Bryan County, South Dakota, could have had significant indirect consequences for the Bryan County Ambulance service, even without PSA’s systems being directly targeted. The interconnected nature of healthcare systems means that a disruption at one point can create ripples throughout the entire network.The ambulance service’s reliance on electronic health records (EHRs), communication systems, and other digital infrastructure makes it vulnerable to collateral damage from a ransomware attack on a partner organization.
For example, if PSA’s EHR system contained patient information crucial for ambulance personnel responding to emergencies, a ransomware attack could significantly impede the ambulance service’s ability to provide timely and effective care.
Indirect Impacts on Ambulance Services
A ransomware attack on PSA could have disrupted ambulance services in several ways. Imagine a scenario where PSA’s patient database, containing critical information such as allergies, medical history, and ongoing treatments, became inaccessible due to encryption. Ambulance crews responding to an emergency involving a PSA patient might find themselves lacking essential information, potentially leading to delays in treatment or incorrect medical decisions.
Furthermore, if PSA used a shared electronic communication system with the ambulance service, a ransomware attack could disrupt dispatch procedures, hindering communication between dispatchers and paramedics. Another potential scenario is the disruption of billing and insurance processes. If the ambulance service relied on PSA’s systems for patient billing, a ransomware attack could lead to delays in reimbursements and financial difficulties.
This indirect impact, while not directly related to patient care, could still significantly affect the ambulance service’s operational capabilities.
Emergency Response Protocols
Effective emergency response protocols are crucial for mitigating the impact of a ransomware attack. These protocols should include robust data backup and recovery procedures, a clear incident response plan, and regular cybersecurity training for all staff. The plan should Artikel steps to be taken in case of a system outage, including the establishment of alternative communication channels and procedures for accessing critical patient information through offline methods.
This could include utilizing paper-based records, accessing backup systems, or establishing communication through alternative means, such as phone calls or radio. Regular security audits and penetration testing can identify vulnerabilities before they can be exploited. Furthermore, the plan should specify how to coordinate with other healthcare providers, such as hospitals and other ambulance services, to ensure continuity of care during a disruption.
A well-defined protocol for communicating with patients and their families about any service disruptions is also essential.
Coordinated Response Between PSA and Bryan County Ambulance
A coordinated response between PSA and Bryan County Ambulance is essential to minimize the effects of future cyberattacks. This could involve sharing information about cybersecurity best practices, participating in joint cybersecurity training exercises, and developing a mutual aid agreement to provide backup support in case of an incident. Regular communication and information sharing are crucial to quickly identify and respond to any potential threats.
Joint disaster recovery planning, including establishing alternative communication channels and data backup procedures, would help ensure the continuity of patient care even in the event of a ransomware attack. This could involve establishing a shared, secure communication platform and regularly testing alternative methods of data access. Establishing a clear chain of command and communication protocols would also be essential in coordinating a rapid and effective response.
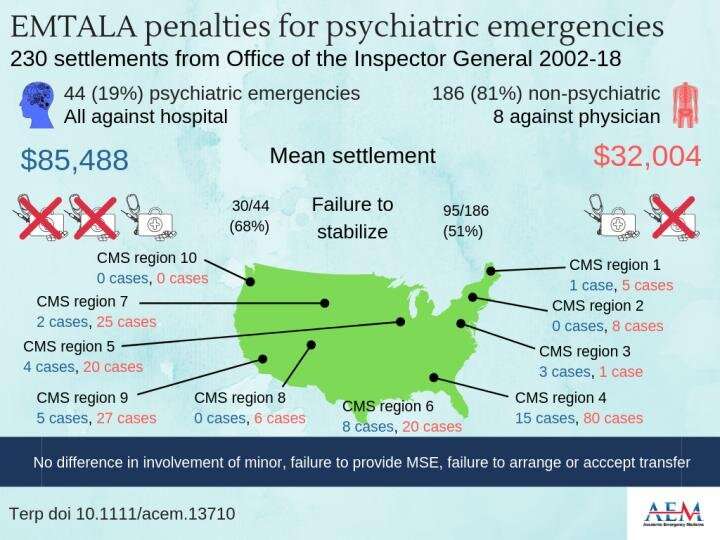
Broader Implications of the Incident

Source: co.nz
The ransomware attack on Plastic Surgery Associates and the subsequent involvement of Bryan County Ambulance in South Dakota highlights a critical vulnerability within the healthcare system. The incident’s ramifications extend far beyond the immediate financial and operational disruptions, raising significant ethical, security, and training concerns for healthcare providers across the state and beyond. This necessitates a thorough examination of the broader implications to prevent future occurrences and mitigate potential damage.The release of patient data following a ransomware attack presents a complex ethical dilemma.
Balancing the need for transparency with the imperative to protect patient privacy is paramount. The potential for identity theft, medical fraud, and emotional distress caused by the unauthorized disclosure of sensitive health information is substantial. Healthcare providers must grapple with the ethical responsibility to notify affected individuals promptly and transparently, while also adhering to relevant privacy regulations like HIPAA.
Failure to do so can lead to legal repercussions and irreparable damage to public trust.
Ethical Considerations Surrounding Patient Data Release
The ethical considerations surrounding the release of patient data are multifaceted. The decision to release data, even partially, must be carefully weighed against the potential harms to patients. This requires a thorough risk assessment, taking into account the sensitivity of the data compromised, the likelihood of misuse, and the availability of mitigation strategies. Open communication with patients and regulatory bodies is essential, ensuring transparency and accountability in the handling of sensitive information.
Furthermore, the ethical framework should encompass not only the immediate consequences but also the long-term impact on patient trust and the provider’s reputation.
Comparison of Security Measures Employed by Healthcare Providers in South Dakota
While specific security measures employed by individual healthcare providers in South Dakota are often confidential for competitive and security reasons, general observations can be made. Larger healthcare systems typically have more robust cybersecurity infrastructure, including dedicated IT security teams and advanced threat detection systems. Smaller practices, like Plastic Surgery Associates, may rely on less sophisticated solutions, potentially leaving them more vulnerable to ransomware attacks.
The disparity in resources and expertise contributes to a heterogeneous security landscape, making a consistent and comprehensive approach challenging. This inconsistency underscores the need for collaborative efforts and government initiatives to enhance cybersecurity across the board.
Importance of Cybersecurity Training for Healthcare Professionals
Cybersecurity training is no longer a luxury but a necessity for healthcare professionals. Human error remains a significant factor in many ransomware attacks, often stemming from phishing scams or accidental clicks on malicious links. Comprehensive training programs should cover topics such as phishing awareness, password management, secure email practices, and incident response protocols. Regular training sessions, reinforced with simulated phishing attacks and scenario-based exercises, can significantly improve employee vigilance and reduce the risk of successful ransomware attacks.
Investing in effective training is a cost-effective measure compared to the potential financial and reputational damage of a ransomware incident.
Best Practices for Enhancing Cybersecurity Posture
A robust cybersecurity posture requires a multi-layered approach. The following best practices are crucial for healthcare organizations:
- Implement Multi-Factor Authentication (MFA): MFA adds an extra layer of security by requiring multiple forms of authentication, making it significantly harder for attackers to gain unauthorized access.
- Regularly Update Software and Systems: Outdated software contains vulnerabilities that attackers can exploit. Regular patching and updates are essential to minimize these risks.
- Conduct Regular Security Audits and Penetration Testing: Regular assessments can identify weaknesses in the system’s security and allow for proactive mitigation of vulnerabilities.
Illustrative Examples of Data Breach Impact: Hhs Ransomware Settlements Plastic Surgery Assciates South Dakota Bryan County Ambulance
The ransomware attack on Plastic Surgery Associates and Bryan County Ambulance had far-reaching consequences, extending beyond the immediate disruption of services. The stolen data directly impacted patients, leading to emotional distress, financial losses, and long-term reputational damage for the involved organizations. Let’s examine some hypothetical scenarios to illustrate the severity of these impacts.
Emotional Distress from Data Compromise
Imagine Sarah Miller, a patient of Plastic Surgery Associates, whose medical history, including sensitive details about a recent surgery and ongoing medication, was compromised in the ransomware attack. Upon learning of the breach, Sarah experienced significant anxiety and fear. She worried about the potential misuse of her personal health information, the possibility of identity theft, and the potential for discrimination from insurance companies or employers.
The HHS ransomware settlements involving Plastic Surgery Associates in South Dakota and Bryan County Ambulance highlight the vulnerability of healthcare data. Thinking about effective data security, I was reminded of a recent article about salesforce healthcare ai sean kennedy and its potential to improve patient data management. Perhaps advanced AI solutions like those discussed could help prevent future breaches and minimize the impact of ransomware attacks on vulnerable healthcare providers like those in the South Dakota settlements.
This anxiety manifested as sleepless nights, increased irritability, and a general feeling of vulnerability and helplessness. The violation of her privacy caused considerable emotional distress, impacting her mental well-being and requiring her to seek professional counseling.
Financial Repercussions from Identity Theft
Consider John Smith, another patient whose information was stolen. In this scenario, John’s identity was used to open fraudulent credit accounts, resulting in significant debt. He spent countless hours disputing charges, contacting credit bureaus, and attempting to repair his damaged credit score. The financial burden extended beyond the immediate debt; John also faced increased interest rates on loans and difficulties securing future credit.
The time and effort spent rectifying the situation caused a significant disruption to his personal and professional life, resulting in lost income and added stress. The cost of credit monitoring and legal assistance further compounded his financial losses.
Long-Term Reputational Damage
The ransomware attack inflicted considerable damage to the reputations of both Plastic Surgery Associates and Bryan County Ambulance. Patients lost trust in the organizations’ ability to protect their sensitive information, leading to a decline in patient numbers and a negative impact on future revenue. The negative publicity surrounding the incident, amplified by media coverage and online discussions, further eroded public confidence.
Repairing this damage will require significant investment in cybersecurity infrastructure, transparency with patients, and a concerted effort to rebuild trust over an extended period. This reputational harm could affect future business opportunities and partnerships.
Visual Representation of the Chain of Events
Imagine a branching diagram. At the top is the “Ransomware Attack.” From this central point, three main branches extend downwards. The first branch leads to “Patient Data Breach,” which further branches into “Emotional Distress” (illustrating Sarah’s experience), and “Financial Repercussions” (illustrating John’s experience). The second branch extends to “Organizational Disruption,” branching into “Service Interruption,” “Financial Losses,” and “Legal Costs.” The third branch leads to “Reputational Damage,” branching into “Loss of Patient Trust,” “Negative Publicity,” and “Difficulty Securing Funding/Partnerships.” Each end point represents a significant negative consequence stemming from the initial ransomware attack, illustrating the cascading effect of the incident.
Summary
The South Dakota ransomware attack serves as a stark reminder of the critical need for robust cybersecurity measures in healthcare, especially in rural areas. The financial burden on the HHS, the legal ramifications for involved parties, and the lasting impact on patient trust underscore the gravity of the situation. Moving forward, a collaborative approach – improved cybersecurity training, enhanced data protection protocols, and coordinated emergency response strategies – is crucial to prevent similar incidents and safeguard the health and well-being of communities across the nation.
This isn’t just a healthcare problem; it’s a public safety issue.
FAQ Compilation
What specific types of data were likely compromised in the Plastic Surgery Associates breach?
Potentially, patient medical records (including sensitive health information), financial data (billing information, insurance details), and employee information could have been compromised.
What kind of financial burden did the HHS face due to this settlement?
The exact amount isn’t publicly available, but ransomware settlements can cost millions, impacting the HHS budget and potentially diverting funds from other essential healthcare services.
What are the long-term consequences for Plastic Surgery Associates’ reputation?
A data breach can severely damage a healthcare provider’s reputation, leading to loss of patients, decreased trust, and potential legal actions.
How could Bryan County Ambulance have been indirectly affected?
If Plastic Surgery Associates’ systems were used for patient transfers or communication, a ransomware attack could disrupt these processes, delaying ambulance response times or hindering communication with other healthcare facilities.