
Is It Safe to Get Preterm Cesarean Sections?
Is it safe to get pre term cesarean sections – Is it safe to get preterm Cesarean sections? That’s the big question many expectant parents grapple with, especially when faced with a premature birth. This isn’t a simple yes or no answer, unfortunately. Preterm Cesarean sections, while sometimes life-saving, carry risks for both mother and baby. We’ll delve into the potential complications, explore the medical necessities that might necessitate this procedure, and examine alternatives to help you navigate this complex decision with a clearer understanding.
The decision to have a preterm Cesarean is deeply personal and should always be made in consultation with your medical team. Weighing the potential risks against the benefits is crucial. This post aims to provide you with the information you need to have an informed conversation with your doctor and feel empowered in your choices.
Maternal Risks of Preterm Cesarean Sections
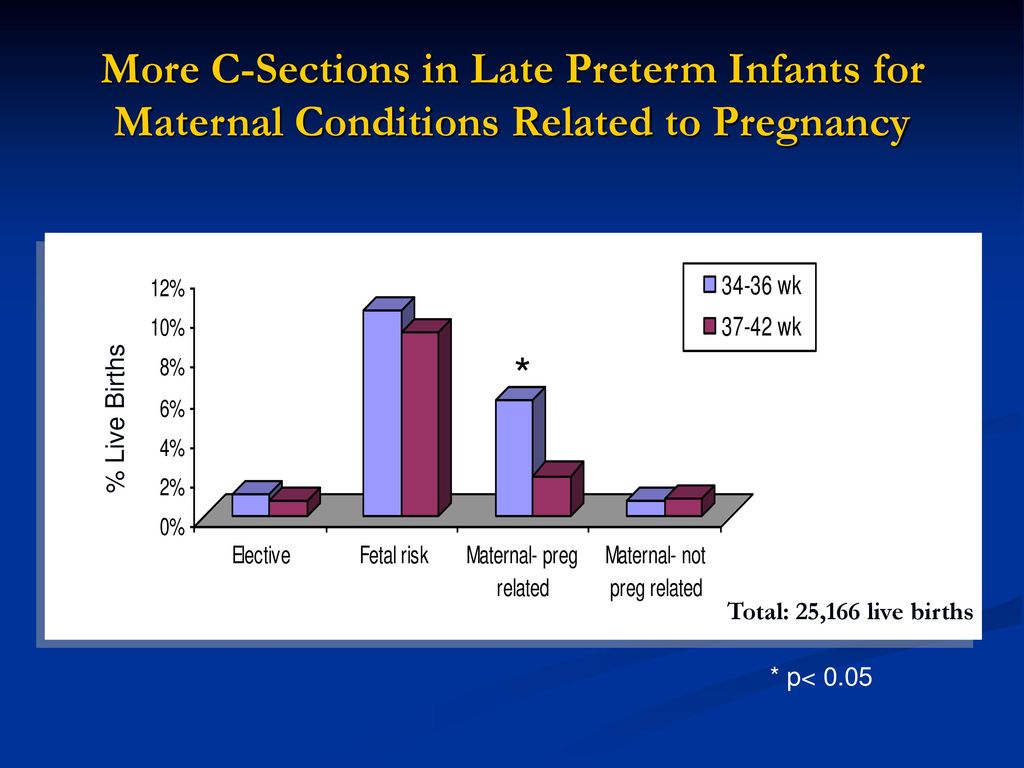
Source: slideplayer.com
Preterm Cesarean sections, while sometimes life-saving for both mother and baby, carry significant risks for the mother. These risks are amplified compared to term Cesarean sections and vaginal deliveries, primarily due to the physiological immaturity of both the mother and the fetus. Understanding these potential complications is crucial for informed decision-making during pregnancy and labor.
Increased Risk of Postpartum Hemorrhage
Preterm Cesarean deliveries are associated with a heightened risk of postpartum hemorrhage (PPH), defined as blood loss exceeding 500ml after vaginal delivery or 1000ml after Cesarean delivery. Several factors contribute to this increased risk. The uterus may not contract effectively after delivery, leading to excessive bleeding. Additionally, preterm pregnancies often involve placental abnormalities that can increase the risk of bleeding.
Furthermore, the use of medications to manage preterm labor can also impact blood clotting mechanisms. Effective management strategies include prompt identification of PPH risk factors, meticulous surgical technique during the Cesarean section, and the ready availability of uterotonics (medications that stimulate uterine contractions) and blood products.
Potential for Infection
Preterm Cesarean sections increase the mother’s risk of various infections, including endometritis (infection of the uterine lining), wound infections, and urinary tract infections (UTIs). Several reasons contribute to this increased susceptibility. Prolonged surgical procedures, potential for tissue damage, and compromised immune function due to the stress of preterm labor and delivery all play a role. Prophylactic antibiotics are commonly administered before surgery to help mitigate this risk.
However, meticulous surgical technique, diligent postoperative wound care, and prompt treatment of any signs of infection are also critical. The severity of these infections can range from mild to life-threatening, highlighting the importance of vigilant monitoring and prompt medical intervention.
Recovery Time Compared to Term Vaginal Delivery
Recovery from a preterm Cesarean section is generally longer and more challenging than recovery from a term vaginal delivery. The physiological stress of preterm labor and delivery, combined with the major surgery involved in a Cesarean section, contribute to a prolonged recovery period. Mothers may experience more intense pain, require longer hospital stays, and need more extensive postpartum support compared to mothers who have a term vaginal delivery.
The body’s healing process is also influenced by the prematurity of the pregnancy, with potentially slower tissue repair and greater susceptibility to complications. Furthermore, the emotional toll of having a preterm baby adds another layer of complexity to the recovery process.
Long-Term Health Consequences for the Mother
The following table summarizes potential long-term health consequences for mothers following preterm Cesarean sections:
| Risk Factor | Description | Severity | Management |
|---|---|---|---|
| Adhesions | Formation of scar tissue that can cause pain and bowel obstruction. | Variable; can range from mild discomfort to severe complications requiring surgery. | Pain management, regular follow-up, surgery if necessary. |
| Chronic Pelvic Pain | Persistent pain in the pelvic region, potentially related to adhesions, nerve damage, or other factors. | Variable; can significantly impact quality of life. | Pain management, physical therapy, surgery in severe cases. |
| Post-traumatic Stress Disorder (PTSD) | Development of PTSD related to the stress of preterm labor, delivery, and neonatal intensive care unit (NICU) stay. | Variable; can range from mild anxiety to severe mental health challenges. | Therapy, support groups, medication. |
| Increased Risk of Subsequent Preterm Labor | Higher chance of experiencing preterm labor in future pregnancies. | Moderate; can lead to repeated preterm deliveries. | Close monitoring during subsequent pregnancies, preventative strategies. |
Fetal Risks of Preterm Cesarean Sections

Source: slidesharecdn.com
Preterm Cesarean sections, while sometimes necessary to save the mother’s life or the baby’s, carry significant risks for the infant. These risks are amplified by the fact that the baby’s lungs, brain, and other organs are not yet fully developed. Understanding these risks is crucial for informed decision-making in high-risk pregnancies.
Respiratory Problems in Premature Infants Born via Cesarean Section
Premature infants, regardless of delivery method, are at increased risk of respiratory distress syndrome (RDS). This is because their lungs haven’t fully developed the surfactant needed to keep the air sacs inflated. However, some studies suggest that Cesarean delivery, particularly elective preterm Cesarean sections, may slightly increase the risk of RDS compared to vaginal delivery at the same gestational age.
This may be due to the lack of the natural squeezing action during vaginal delivery which helps clear fluid from the baby’s lungs. The severity of RDS can range from mild breathing difficulties to life-threatening respiratory failure requiring mechanical ventilation.
Neonatal Intensive Care Unit (NICU) Admission Following Preterm Cesarean Section, Is it safe to get pre term cesarean sections
The likelihood of NICU admission is significantly higher for preterm infants born via Cesarean section. This is because these infants often require specialized medical care to address respiratory problems, feeding difficulties, temperature instability, and other complications associated with prematurity. The length of stay in the NICU can vary greatly depending on the infant’s gestational age, birth weight, and the presence of any complications.
A longer NICU stay translates to increased healthcare costs and potential emotional stress for the parents.
Neurological Complications Associated with Preterm Cesarean Delivery
Preterm infants are at an increased risk of various neurological complications, including intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), and cerebral palsy. While the exact relationship between preterm Cesarean delivery and these complications is complex and not fully understood, some research suggests a possible association, particularly for very preterm infants. These neurological complications can have long-lasting effects on the infant’s cognitive and motor development.
For example, IVH, bleeding in the brain’s ventricles, can lead to developmental delays or disabilities.
Infant Mortality Rates Related to Preterm Cesarean Sections
While Cesarean sections can be life-saving in certain situations, studies have shown a correlation between preterm Cesarean sections and increased infant mortality rates, particularly when performed before 34 weeks of gestation. The increased risk is likely multifactorial, encompassing the complications discussed above, such as respiratory distress and neurological issues. The exact mortality rate varies depending on factors such as gestational age, maternal health, and the presence of other complications.
It’s crucial to remember that this increased risk does not negate the potential life-saving benefits of a Cesarean section in certain high-risk pregnancies.
Potential Short-Term and Long-Term Effects on Infant Development
The following points Artikel potential short-term and long-term effects on an infant’s development after a preterm Cesarean section. It’s important to remember that not all preterm infants born via Cesarean section will experience these complications, and the severity of any complications can vary widely.
- Short-term effects: Respiratory distress, difficulty feeding, temperature instability, jaundice, infection, and prolonged NICU stay.
- Long-term effects: Developmental delays (cognitive, motor, or language), cerebral palsy, learning disabilities, vision or hearing problems, and behavioral problems.
Medical Indications for Preterm Cesarean Sections
Preterm Cesarean sections, while carrying inherent risks, are sometimes medically necessary to safeguard both the mother’s and the baby’s well-being. These interventions are not taken lightly and are always made after careful consideration of the potential benefits against the risks involved. The decision to proceed is based on a thorough assessment of the maternal and fetal condition, and often involves a multidisciplinary team of healthcare professionals.
Fetal Distress as an Indication for Preterm Cesarean Section
Fetal distress, characterized by abnormalities in the fetal heart rate pattern during labor, is a critical indication for immediate intervention, often including a Cesarean section. This distress can manifest as decelerations (slowing of the heart rate), accelerations (sudden increases in heart rate), or a lack of variability (consistent changes in the heart rate). These changes can signal that the fetus is not receiving adequate oxygen, potentially leading to hypoxia (lack of oxygen) and brain damage.
The severity and duration of the distress, along with the mother’s overall condition, inform the decision to perform a Cesarean section. For example, recurrent late decelerations (heart rate slowing that occurs after a uterine contraction) that don’t recover quickly can indicate a critical lack of oxygen to the fetus, prompting immediate action.
Maternal Health Conditions Requiring Preterm Cesarean Section
Several maternal health conditions can necessitate a preterm Cesarean section to protect the mother’s health and potentially the fetus. These include severe preeclampsia (high blood pressure during pregnancy), eclampsia (seizures associated with preeclampsia), placental abruption (premature separation of the placenta from the uterine wall), uterine rupture (tear in the uterine wall), and severe hemorrhage (heavy bleeding). In these cases, the risks associated with continuing the pregnancy often outweigh the risks of a preterm Cesarean section.
For instance, a severe placental abruption can lead to rapid blood loss for both the mother and the baby, making immediate delivery via Cesarean section life-saving.
Comparison of Medical Indications for Preterm and Term Cesarean Sections
While both preterm and term Cesarean sections share some indications, such as fetal distress and maternal complications like severe preeclampsia, the urgency and implications differ significantly. Term Cesareans often involve less immediate risk to the fetus, allowing for more time for assessment and preparation. In contrast, preterm Cesarean sections often require immediate action due to the increased vulnerability of a premature infant and the potential for rapid deterioration in the maternal or fetal condition.
The decision-making process is more time-sensitive in preterm cases, demanding swift action to minimize risks.
So, is it safe to get a preterm Cesarean section? It’s a complex question with many factors influencing the decision. Thinking about the risks involved reminds me of Karishma Mehta’s recent decision to freeze her eggs – check out the article on the risks associated with that procedure: karishma mehta gets her eggs frozen know risks associated with egg freezing.
Just like egg freezing, preterm Cesareans carry potential risks, but sometimes it’s the safest option for both mother and baby. Weighing those risks is crucial.
Decision-Making Flowchart for Preterm Cesarean Section
The decision to perform a preterm Cesarean section is complex and relies on a thorough assessment of both maternal and fetal well-being. A simplified flowchart would look like this:[Imagine a flowchart here. It would begin with a box labeled “Maternal and Fetal Assessment”. This would branch to two boxes: “Maternal Condition Stable/Fetal Condition Stable” and “Maternal Condition Unstable/Fetal Condition Unstable”.
The “Stable” branch would lead to a box labeled “Continue Monitoring/Vaginal Delivery Considered”, potentially with another branch to “Cesarean Section” if conditions deteriorate. The “Unstable” branch would directly lead to a box labeled “Cesarean Section”. From the “Cesarean Section” box, arrows would point to “Post-operative Care” for both mother and baby.]This flowchart represents a simplified process. In reality, the decision involves multiple factors, continuous monitoring, and the expertise of a multidisciplinary team, including obstetricians, neonatologists, and anesthesiologists.
Alternatives to Preterm Cesarean Sections: Is It Safe To Get Pre Term Cesarean Sections
Preterm birth, defined as birth before 37 weeks of gestation, presents significant challenges for both mother and baby. While Cesarean section is sometimes necessary to address immediate threats, exploring alternatives is crucial for optimizing maternal and fetal outcomes. This section examines various strategies aimed at delaying preterm delivery and potentially avoiding the need for a preterm Cesarean.Expectant Management in Preterm PregnanciesExpectant management involves close monitoring of the mother and fetus without immediate intervention, aiming to prolong pregnancy until fetal maturity improves.
This approach carefully weighs the risks of continued pregnancy against the risks of premature delivery. The decision to pursue expectant management is highly individualized, considering factors such as gestational age, fetal lung maturity, presence of infection, and maternal health.
Benefits and Risks of Expectant Management
Expectant management offers the potential to gain valuable time for fetal lung development, reducing the risk of respiratory distress syndrome (RDS) in the newborn. It also avoids the immediate risks associated with Cesarean section, such as infection, bleeding, and potential long-term complications. However, expectant management carries its own set of risks. These include the potential for worsening of underlying maternal or fetal conditions, placental abruption, or the development of severe complications requiring emergency intervention, including Cesarean section.
The potential benefits must be carefully weighed against these risks in each individual case. For example, a mother with a stable preterm pregnancy at 34 weeks might benefit from expectant management, allowing for further fetal maturation, whereas a mother with signs of chorioamnionitis (infection of the amniotic sac) at 28 weeks would likely require immediate intervention.
The Role of Tocolytics
Tocolytics are medications used to suppress uterine contractions and delay preterm labor. These medications buy valuable time to allow for the administration of corticosteroids to enhance fetal lung maturity or for transfer to a higher-level care facility. Common tocolytics include magnesium sulfate, indomethacin, and nifedipine. Each medication has its own set of potential side effects that must be carefully considered.
For instance, magnesium sulfate can cause side effects like nausea, flushing, and low blood pressure, while indomethacin may affect fetal circulation. The decision to use tocolytics depends on several factors, including gestational age, the presence of contractions, and the overall maternal and fetal condition. It’s important to note that tocolytics do not prevent preterm birth indefinitely; their primary role is to delay delivery for a limited period, allowing for other interventions.
The Use of Corticosteroids
Corticosteroids, such as betamethasone or dexamethasone, are administered to the mother to accelerate fetal lung maturity. This significantly reduces the risk of respiratory distress syndrome (RDS) in premature infants. Corticosteroids are typically given in two doses, 24 hours apart, and their benefits are most pronounced when administered between 24 and 34 weeks of gestation. While generally safe, corticosteroids can have potential side effects, including maternal hyperglycemia and increased risk of infection.
However, the benefits of reducing neonatal RDS greatly outweigh these risks.
Comparison of Expectant Management and Immediate Cesarean Section
The decision between expectant management and immediate Cesarean section is complex and depends on a multitude of factors, including gestational age, fetal status, maternal health, and the presence of any complications. A premature infant born at 24 weeks gestation faces significantly higher risks than one born at 32 weeks. Similarly, the presence of severe maternal complications, such as pre-eclampsia or placental abruption, may necessitate immediate intervention.
In situations where there is a significant risk of fetal compromise or maternal deterioration, immediate Cesarean section is often the safest course of action. Conversely, in stable pregnancies closer to term with favorable fetal conditions, expectant management may be a reasonable approach.
Management Strategies for Preterm Labor: A Comparison
| Management Strategy | Success Rate (Variable, depends on many factors) | Potential Risks |
|---|---|---|
| Expectant Management | Highly variable, depends on gestational age and underlying conditions; may range from successful prolongation to emergency Cesarean. | Fetal distress, placental abruption, infection, maternal complications. |
| Tocolysis with Magnesium Sulfate | May delay delivery for a few hours to days, but does not prevent preterm birth. | Maternal hypotension, nausea, vomiting, flushing, muscle weakness. |
| Tocolysis with Indomethacin | Similar to magnesium sulfate in delaying delivery. | Fetal complications (oligohydramnios, patent ductus arteriosus). |
| Corticosteroid Administration | Reduces the risk of RDS in the newborn, but does not prevent preterm birth. | Maternal hyperglycemia, increased risk of infection. |
| Immediate Cesarean Section | Immediate delivery, addresses immediate threats to mother and/or fetus. | Surgical risks (infection, bleeding, injury), maternal and neonatal complications. |
Post-Operative Care Following Preterm Cesarean Section
The recovery period after a preterm Cesarean section is crucial for both mother and baby. It requires a multifaceted approach encompassing pain management, close monitoring for complications, and specialized care for the premature infant. The intensity and duration of this post-operative care vary depending on the gestational age of the baby, the mother’s overall health, and any complications arising during or after the surgery.
Pain Management Strategies
Effective pain management is paramount for a mother’s comfort and recovery after a preterm Cesarean section. The pain experienced can be significant due to the incision, uterine contractions, and potential surgical complications. A multimodal approach, often involving a combination of analgesics, is typically employed. This might include intravenous opioids initially, transitioning to oral pain relievers such as NSAIDs or acetaminophen as tolerated.
Epidural analgesia can also be used, providing continuous pain relief. Regular pain assessments are essential to adjust the medication regimen and ensure adequate pain control. Non-pharmacological methods, such as positioning techniques, skin-to-skin contact with the baby (if the baby’s condition allows), and relaxation exercises, can complement pharmacological approaches, contributing to a holistic pain management strategy.
Monitoring for Potential Complications
Post-operative monitoring focuses on detecting and managing potential complications in both mother and baby. For the mother, this includes vigilant observation for signs of infection (fever, redness, swelling at the incision site), bleeding (excessive vaginal discharge, decreased blood pressure), and thromboembolic events (deep vein thrombosis, pulmonary embolism). Regular vital signs monitoring, wound assessment, and blood tests are essential. For the baby, monitoring includes assessing respiratory function, temperature regulation, feeding tolerance, and overall growth and development.
Close observation for signs of infection, respiratory distress syndrome, or other complications associated with prematurity is crucial. The frequency of monitoring will depend on the gestational age and the baby’s health status.
Breastfeeding and Newborn Care
Breastfeeding a preterm infant presents unique challenges and benefits. Colostrum, the initial breast milk, is rich in antibodies and essential nutrients crucial for the baby’s immune system and development. Skin-to-skin contact, often called kangaroo care, can help regulate the baby’s temperature, heart rate, and oxygen saturation. However, preterm infants may require assistance with latching and feeding, potentially necessitating supplementation with breast milk or formula via a feeding tube.
Specialized neonatal care units provide support and guidance on breastfeeding techniques and strategies for optimizing milk production. Educating mothers about the importance of breastfeeding and providing appropriate support is critical for successful breastfeeding initiation and continuation.
Wound Care and Infection Prevention
Proper wound care is crucial to prevent infection and promote healing. The incision site is typically assessed regularly for signs of infection, such as redness, swelling, increased pain, or drainage. The dressing is changed according to the healthcare provider’s instructions, often involving the use of sterile technique. The mother is educated on proper hygiene practices, including washing her hands before and after touching the incision site.
Antibiotics are often administered prophylactically to reduce the risk of infection. In cases of infection, appropriate antibiotic treatment is promptly initiated. Regular follow-up appointments are scheduled to monitor wound healing and address any concerns.
Long-Term Effects on Mother and Child
Preterm Cesarean sections, while sometimes life-saving, can have lasting impacts on both the mother and the child. Understanding these potential long-term effects is crucial for informed decision-making and effective post-operative care. This section will explore the physical, emotional, and developmental consequences for both parents and their child.
Preterm Cesarean sections are a serious medical decision, weighing the risks against the benefits for both mother and baby. It’s a completely different realm from considering health risks later in life, like the fascinating research on whether an eye test can detect dementia risk, as explored in this article: can eye test detect dementia risk in older adults.
Understanding the long-term health implications, however, is crucial in both scenarios, highlighting the importance of thorough medical consultations before making such life-altering choices.
Long-Term Physical Effects on the Mother
Mothers who undergo preterm Cesarean sections may experience various long-term physical effects. These can include chronic pelvic pain, increased risk of future complications in subsequent pregnancies (such as placenta previa or accreta), and potential issues with bowel or bladder function. Scar tissue from the incision can also lead to discomfort or limitations in physical activity. Furthermore, some women experience ongoing pain or numbness around the incision site.
The severity of these effects varies greatly depending on individual factors, the complexity of the surgery, and the quality of post-operative care.
Long-Term Emotional Effects on the Mother
The emotional toll of a preterm Cesarean section can be significant. The stress of a premature birth, coupled with the physical recovery from surgery, can contribute to postpartum depression and anxiety. Feelings of guilt, inadequacy, and grief over not experiencing a vaginal delivery are also common. These emotional challenges can impact the mother’s ability to bond with her baby and navigate the demands of parenthood.
Access to adequate support systems, including mental health professionals, is vital for managing these emotional consequences.
Long-Term Developmental Effects on the Child
Premature infants born via Cesarean section, regardless of the reason for the procedure, face a heightened risk of several long-term developmental challenges. These can include respiratory problems, neurodevelopmental delays, cerebral palsy, learning disabilities, and vision or hearing impairments. The severity of these effects is often correlated with the degree of prematurity. Early intervention programs and ongoing monitoring are crucial in mitigating these risks and supporting the child’s development.
For example, a child born at 24 weeks gestation will likely face more significant challenges than a child born at 34 weeks.
Psychological Impact on Parents
The psychological impact on parents following a preterm Cesarean section is multifaceted. The experience can be profoundly stressful, leading to anxiety, depression, and relationship strain. The prolonged hospital stay, intensive care requirements for the baby, and the emotional rollercoaster of facing potential health complications for the child significantly affect parental well-being. Open communication between partners, seeking professional support, and joining support groups for parents of premature infants can be invaluable coping mechanisms.
Comparison of Long-Term Outcomes: Cesarean vs. Vaginal Delivery (Preterm)
While vaginal delivery is generally preferred for full-term pregnancies, the decision between Cesarean and vaginal delivery for preterm births is complex and often medically driven. Comparing long-term outcomes directly is challenging due to the confounding factors of prematurity itself. However, studies suggest that some long-term risks, such as respiratory issues and neurodevelopmental delays, may be slightly higher for preterm infants born via Cesarean section, though this difference isn’t always significant and depends heavily on gestational age and the specific medical reasons for the Cesarean.
In many cases, a Cesarean section is the safer option for both mother and baby, despite the potential long-term considerations.
So, is it safe to get a preterm Cesarean section? It’s a complex question, depending heavily on the specific circumstances. Understanding the risks involved is crucial, and sometimes those risks mirror broader health concerns; for example, pre-existing conditions like high blood pressure, a known risk factor for preterm birth, are also listed among the risk factors that make stroke more dangerous.
Therefore, a thorough assessment of maternal health is essential before deciding on a preterm C-section to ensure both mom and baby are as safe as possible.
Long-Term Effects: Summary Table
| Effect | Mother | Child | Management Strategies |
|---|---|---|---|
| Physical | Chronic pelvic pain, increased risk of future pregnancy complications, bowel/bladder issues, incision site discomfort | Respiratory problems, neurodevelopmental delays, cerebral palsy, learning disabilities, vision/hearing impairments | Physical therapy, pain management, medication, ongoing medical monitoring |
| Emotional | Postpartum depression/anxiety, guilt, inadequacy, grief | (Indirect impact through parental stress) | Therapy, support groups, counseling, strong support network |
| Developmental | (Indirect impact through stress and physical recovery) | Developmental delays, learning difficulties, behavioral issues | Early intervention programs, specialized education, ongoing monitoring |
Final Review
Source: plasticsurgeryistanbul.net
Ultimately, the decision regarding a preterm Cesarean section is a highly individualized one. While the procedure carries inherent risks for both mother and child, it can be a life-saving intervention in many circumstances. Understanding these risks, exploring alternative management strategies, and engaging in open communication with your healthcare provider are key to making the best decision for your unique situation.
Remember, informed choices lead to better outcomes, and your health and the well-being of your baby are paramount.
Key Questions Answered
What are the long-term effects on the baby after a preterm Cesarean?
Long-term effects can vary greatly depending on the baby’s gestational age at birth and overall health. Some potential long-term effects include developmental delays, respiratory issues, and increased risk of certain health problems. Regular check-ups and early intervention therapies can help mitigate many of these risks.
How long is the recovery period after a preterm Cesarean?
Recovery time is longer and more challenging than after a term Cesarean. Expect several weeks of significant discomfort and limitations. Full recovery can take several months, and it’s crucial to follow your doctor’s post-operative instructions carefully.
Can I breastfeed after a preterm Cesarean?
Yes, breastfeeding is highly encouraged after a preterm Cesarean, even if your baby is in the NICU. Skin-to-skin contact and expressing colostrum are beneficial even if direct breastfeeding isn’t immediately possible. Your healthcare team can offer support and guidance.
What are the emotional effects on the mother after a preterm Cesarean?
Mothers may experience a range of emotions including anxiety, stress, guilt, and sadness. Postpartum depression is also a possibility. Seeking support from family, friends, or a therapist is important for emotional well-being.
