Medicaid Redeterminations Childrens Coverage Loss & CHIP
Medicaid redeterminations children coverage loss chip – Medicaid redeterminations, children’s coverage loss, and the Children’s Health Insurance Program (CHIP) – these terms might sound bureaucratic, but they represent a very real struggle for many families. The process of renewing Medicaid and CHIP coverage can be confusing and overwhelming, often leading to children losing vital healthcare access. This isn’t just about paperwork; it’s about the health and well-being of our kids, and the ripple effects that losing coverage can have on their lives and futures.
This post delves into the complexities of this system, exploring the challenges families face and highlighting potential solutions.
We’ll examine the statistics surrounding children losing coverage, the disparities affecting certain demographics, and the crucial role CHIP plays in bridging the gap. We’ll also discuss strategies to improve the system, including better communication, simplified applications, and policy changes. Ultimately, the goal is to ensure every child has access to the healthcare they need to thrive.
The Impact of Medicaid Redeterminations on Children
Medicaid redeterminations, the periodic review of eligibility for government healthcare programs, are a crucial but often stressful process for families, particularly those with children. These reviews ensure that only those who qualify continue to receive benefits, but the process itself can be complex and lead to significant disruptions in children’s access to essential healthcare. Understanding the intricacies of this process is key to mitigating its negative impacts.Medicaid redeterminations involve verifying a family’s income, household size, and other eligibility factors.
If a family’s circumstances have changed since their initial application, they may no longer qualify for Medicaid or CHIP (Children’s Health Insurance Program). This can result in a loss of healthcare coverage, leading to delayed or forgone medical care, increased medical debt, and potential negative impacts on a child’s health and well-being. The process often requires significant paperwork, timely submission of documents, and navigating bureaucratic hurdles, all while families juggle daily responsibilities.
Challenges Faced by Families During Redeterminations
The redetermination process presents numerous challenges for families. Many families struggle to gather the necessary documentation, such as proof of income, residency, and identification, particularly if they lack consistent access to technology or reliable transportation. Language barriers can also pose significant obstacles, making it difficult to understand the requirements and complete the forms accurately. Furthermore, the timing of redeterminations can be unpredictable, adding to the stress and uncertainty families already face.
The upcoming Medicaid redeterminations are causing a lot of anxiety, especially concerning potential CHIP coverage loss for children. Efficient documentation is crucial during this process, and that’s where advancements like those detailed in this article about nuance integrates generative ai scribe epic ehrs become incredibly relevant. Streamlining the administrative burden through AI could help ensure kids maintain their vital healthcare coverage during this period of uncertainty.
We need solutions to navigate this complex situation and protect vulnerable children.
For example, a family might receive a renewal notice with a tight deadline while dealing with a job loss or other unexpected life events, making it difficult to prioritize the paperwork and maintain continuous coverage.
Administrative Burdens Impacting Coverage Maintenance
Administrative burdens significantly impact families’ ability to maintain coverage. Complex application forms, confusing instructions, and frequent requests for additional information can overwhelm families, especially those with limited resources or literacy skills. For instance, a family might miss a deadline due to an oversight in the mail or a misunderstanding of the instructions, resulting in a lapse in coverage.
The lack of clear communication and timely responses from government agencies further exacerbates these challenges. A parent might spend hours on hold trying to clarify a question or track down missing documents, time that could be spent working or caring for their children. The sheer volume of paperwork required, coupled with the stress of potential coverage loss, can significantly impact family well-being.
Comparison of Medicaid and CHIP Enrollment
The enrollment processes for Medicaid and CHIP share some similarities but also have key differences. Below is a comparison table illustrating these aspects:
| Feature | Medicaid | CHIP | Notes |
|---|---|---|---|
| Income Eligibility | Based on Federal Poverty Level (FPL), varies by state | Higher than Medicaid’s FPL, varies by state | Specific income limits are determined by each state. |
| Application Process | Online, mail, or in-person | Online, mail, or in-person; often integrated with Medicaid applications | States may offer varying application methods. |
| Documentation Required | Proof of income, residency, identity, and citizenship | Similar to Medicaid; may require additional documentation for children | Specific requirements vary by state and individual circumstances. |
| Renewal Process | Periodic reviews, typically annually | Similar to Medicaid, with periodic renewals | Renewal schedules can vary depending on state regulations. |
Children’s Healthcare Coverage Loss Due to Redeterminations
Source: kff.org
The unwinding of the continuous Medicaid coverage provision enacted during the COVID-19 public health emergency has led to a significant increase in redeterminations, impacting millions of families and, critically, their children’s access to healthcare. This process, where eligibility for Medicaid and CHIP (Children’s Health Insurance Program) is reassessed, has resulted in a substantial number of children losing their crucial health coverage.
Understanding the scope of this issue, its consequences, and the disparities it creates is vital to ensuring all children have access to the care they need.
Number of Children Losing Coverage
Reports from various states show a concerning trend of children losing Medicaid and CHIP coverage following redeterminations. While precise nationwide figures are still emerging and vary by state, initial data suggests hundreds of thousands of children have already lost coverage, with projections indicating this number could rise significantly. For example, early data from [State Name] showed a [Percentage]% increase in children losing coverage in the first [Time Period] of redeterminations.
These numbers highlight the urgent need for support systems and resources to mitigate the impact of these losses.
Health Consequences of Coverage Loss
The loss of healthcare coverage for children can have severe and long-lasting health consequences. Without access to regular check-ups, preventative care, and treatment for illnesses and injuries, children may experience delays in diagnosis and treatment, leading to worsening health conditions. This can particularly impact children with chronic conditions requiring ongoing medical management. For instance, a child with asthma might experience more severe attacks without access to regular medication and monitoring, while a child with a dental issue could suffer from untreated pain and potential infections.
The lack of preventative care can also lead to more serious health problems down the line.
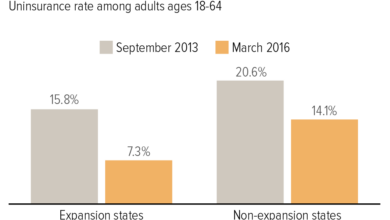
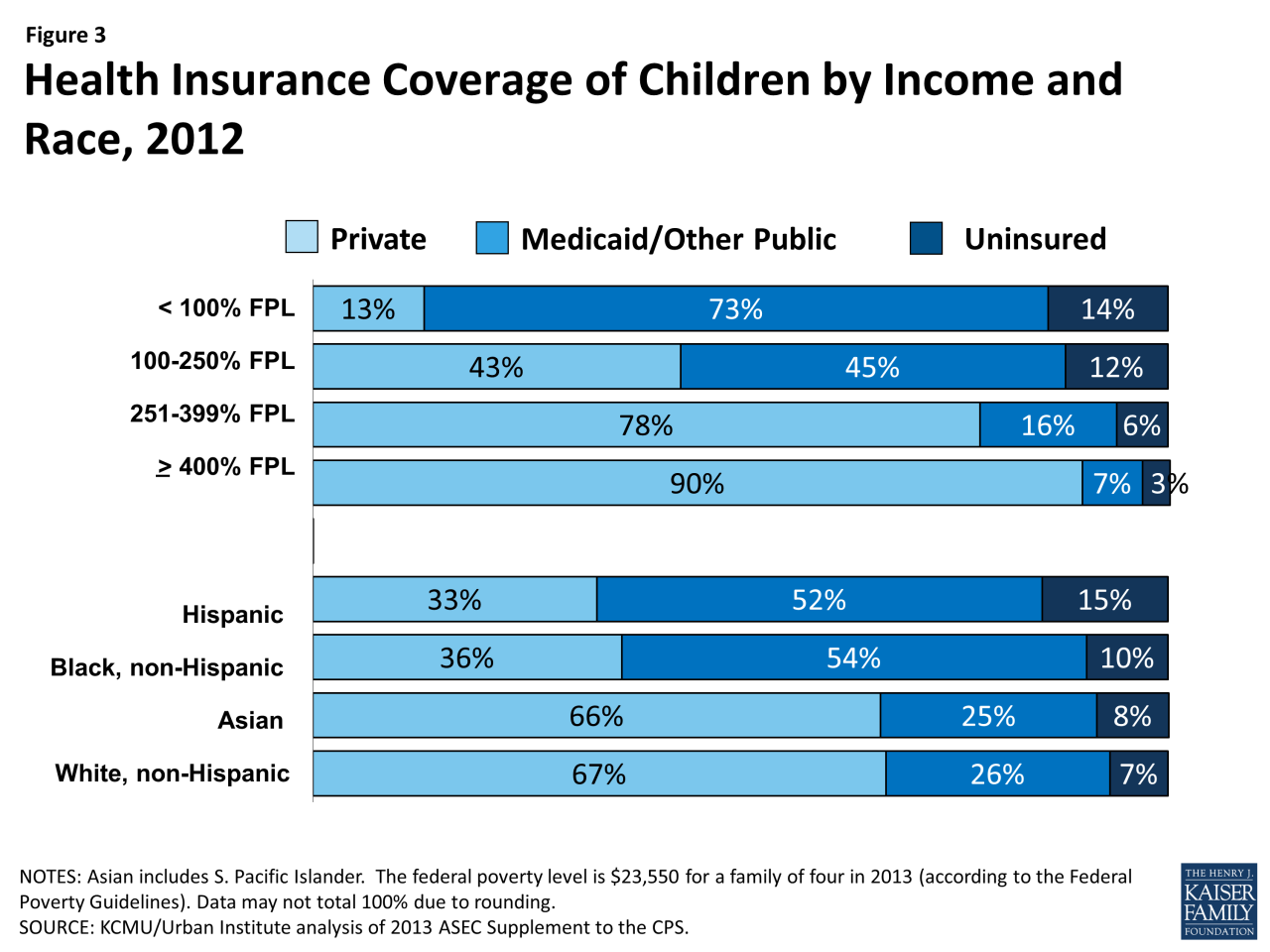
Disparities in Coverage Loss
The impact of Medicaid and CHIP redeterminations is not felt equally across all demographics. Data suggests that children from minority racial and ethnic groups, and those from low-income families, are disproportionately affected by coverage loss. These communities often face systemic barriers to accessing healthcare, including language barriers, lack of transportation, and limited awareness of available resources. This exacerbates existing health inequities and further disadvantages vulnerable children.
For example, studies have shown that [Specific Minority Group] children are [Percentage]% more likely to lose coverage than their [Comparison Group] counterparts.
Resources for Families Facing Coverage Loss
Families facing the loss of Medicaid or CHIP coverage for their children need access to vital resources and support. It is crucial to understand the available options to ensure children continue receiving necessary care.
- State Medicaid Agencies: Contact your state’s Medicaid agency for information about the appeals process, potential eligibility for other programs, and assistance navigating the system.
- CHIP Programs: Explore the Children’s Health Insurance Program (CHIP) in your state, which provides low-cost health coverage to children whose families earn too much to qualify for Medicaid.
- Healthcare Providers: Many healthcare providers offer financial assistance programs or sliding-fee scales to help families afford care.
- Community Health Centers: These centers provide affordable and comprehensive healthcare services to individuals regardless of their insurance status.
- Patient Advocates: Patient advocacy organizations can provide guidance and support in navigating the healthcare system and accessing resources.
The Role of the Children’s Health Insurance Program (CHIP)

Source: pennwatch.org
CHIP, the Children’s Health Insurance Program, plays a vital role in ensuring that children from families who earn too much to qualify for Medicaid but cannot afford private insurance have access to healthcare. It acts as a crucial safety net, bridging the gap between Medicaid and private insurance, and contributing significantly to the overall health and well-being of children across the nation.CHIP provides low-cost health coverage to children in families who earn too much to qualify for Medicaid but cannot afford private health insurance.
The program works in conjunction with Medicaid, offering a comprehensive range of healthcare services, including doctor visits, hospital care, prescription drugs, and dental and vision care. It’s designed to improve children’s health outcomes by ensuring they receive the necessary medical attention to prevent and treat illness and injury.
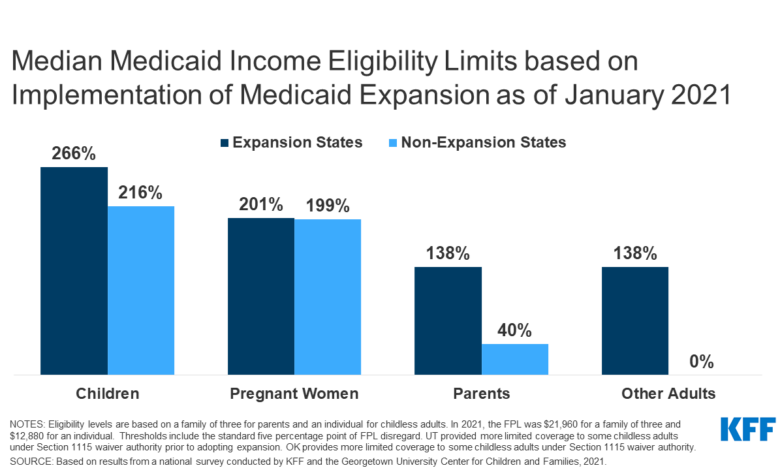
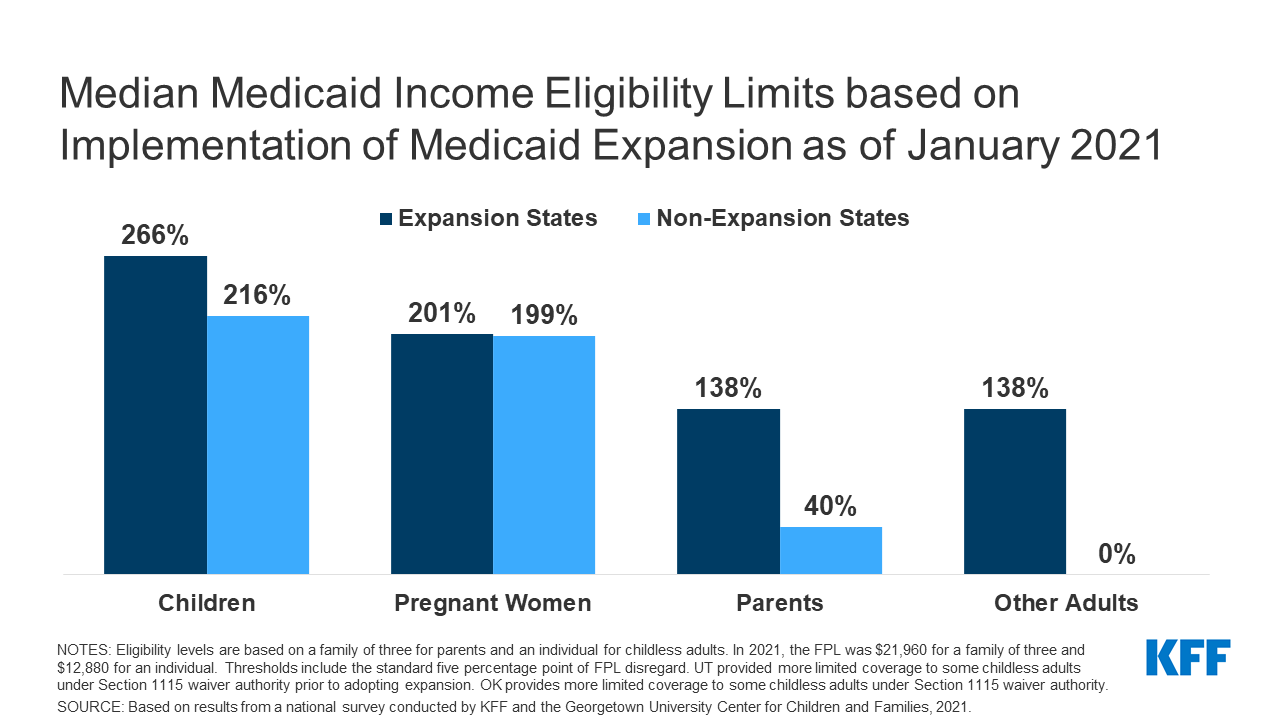
Medicaid and CHIP Eligibility Criteria: A Comparison
Medicaid and CHIP eligibility criteria share some similarities but also have key differences. Both programs consider family income and size, but Medicaid generally has stricter income limits. CHIP often has higher income limits, allowing it to cover children in families who earn slightly more than Medicaid’s thresholds. Additionally, Medicaid eligibility may also consider factors like citizenship status and disability, while CHIP’s requirements may vary slightly by state.
For example, some states may prioritize children from families with very low incomes and expand coverage to families slightly above the federal poverty level. This variation underscores the complexities of navigating eligibility across different states and programs.
Challenges CHIP Faces During Redetermination Periods
Redeterminations, the periodic reviews of eligibility for government assistance programs, present significant challenges for CHIP. During these periods, families must re-submit documentation to prove continued eligibility. Many families face difficulties in providing the necessary paperwork, leading to delays and potential coverage gaps. Changes in family income or household composition can also impact eligibility, resulting in children losing coverage unexpectedly.
Administrative complexities and limited resources in some states exacerbate these challenges, making it difficult to ensure a smooth and efficient redetermination process. This can lead to significant disruptions in children’s access to healthcare, with potential long-term consequences for their health and development.
The Impact of CHIP Funding on Children’s Health Outcomes, Medicaid redeterminations children coverage loss chip
Studies have consistently shown a positive correlation between CHIP coverage and improved children’s health outcomes. For example, research has indicated that CHIP coverage is associated with increased rates of preventative care, such as vaccinations and well-child visits. This leads to earlier detection and treatment of health problems, resulting in fewer hospitalizations and improved overall health. A study published in the journalPediatrics* found that CHIP coverage was associated with a significant reduction in the rate of emergency department visits for children.
While precise figures vary depending on the specific study and population, the overall consensus supports the assertion that CHIP funding demonstrably contributes to better health outcomes for children. The availability of affordable healthcare reduces financial barriers, allowing parents to seek timely medical care for their children, preventing minor health issues from escalating into more serious conditions.
Strategies to Mitigate Children’s Coverage Loss
The loss of Medicaid and CHIP coverage for children during redeterminations is a serious issue with far-reaching consequences. Preventing this loss requires a multi-pronged approach focusing on improved communication, streamlined processes, and supportive policy changes. The strategies Artikeld below aim to minimize disruption to children’s healthcare access and ensure families are equipped to navigate the redetermination process successfully.
The upcoming Medicaid redeterminations are causing serious concern about children losing CHIP coverage. Efficient healthcare management is crucial during this time, and a recent study widespread digital twins healthcare suggests promising solutions. These digital twins could streamline the process and potentially help identify and assist children at risk of losing their vital healthcare coverage, ensuring smoother transitions and preventing unnecessary disruptions.
Improving Communication and Outreach Efforts
Effective communication is crucial to preventing coverage loss. Many families are unaware of the redetermination process or the deadlines involved. A proactive and multi-channel outreach strategy is essential. This could involve sending reminders via mail, text message, and email, utilizing multiple languages to reach diverse communities. Furthermore, partnering with community organizations, schools, and healthcare providers can help disseminate information and provide support to families.
Targeted outreach to vulnerable populations, such as those experiencing homelessness or language barriers, is also critical. For example, a state could implement a system where automated phone calls and text messages are sent to families nearing their renewal date, followed by mailed reminders in multiple languages. These reminders could include clear instructions and contact information for assistance.
Simplifying the Application and Renewal Process
The application and renewal process for Medicaid and CHIP can be complex and burdensome for families. Simplifying this process is key to preventing coverage lapses. This could involve using online portals with user-friendly interfaces, pre-filling applications with existing data, and providing assistance with completing forms. States could also explore options like automatic renewals for families who consistently meet eligibility requirements, reducing the need for frequent re-applications.
For instance, California’s Covered California marketplace uses a simplified online application process that reduces the number of required fields, allowing for faster completion and minimizing errors.
Policy Changes to Reduce Administrative Burdens
Policy changes at the state and federal levels can significantly reduce administrative burdens on families. This could involve extending the renewal period, allowing for more flexible documentation requirements, and providing greater flexibility in verifying income and eligibility. Streamlining data sharing between state agencies can also reduce the need for families to repeatedly submit the same information. For example, a state could implement a policy that allows families to use their tax returns to verify income, eliminating the need for additional documentation.
Federal funding could be allocated to support states in developing and implementing user-friendly online portals and automated systems.
State-Level Initiatives to Prevent Coverage Loss
Several states have implemented innovative initiatives to prevent children from losing their healthcare coverage during redeterminations. The table below summarizes some examples:
| State | Initiative | Description | Impact |
|---|---|---|---|
| California | Simplified Online Application | User-friendly online portal with pre-filled information and reduced paperwork. | Increased enrollment and reduced errors. |
| Oregon | Automated Renewal System | Automatic renewal for families who consistently meet eligibility requirements. | Reduced administrative burden and prevented coverage lapses. |
| Vermont | Community Outreach Programs | Partnerships with community organizations to provide assistance with applications and renewals. | Increased awareness and improved access to assistance. |
| New York | Extended Renewal Periods | Longer renewal periods to provide more time for families to complete the process. | Reduced the likelihood of coverage lapses due to missed deadlines. |
Long-Term Effects of Coverage Loss on Children’s Health
Source: kff.org
Losing health insurance coverage during childhood can have profound and lasting consequences, extending far beyond the immediate lack of access to healthcare. The ripple effects impact a child’s physical and mental well-being, educational trajectory, and ultimately, their future economic prospects. Understanding these long-term effects is crucial for advocating for policies that ensure continuous healthcare access for all children.The absence of consistent healthcare access leads to poorer health outcomes.
Children without insurance are less likely to receive preventative care, resulting in a higher incidence of preventable illnesses and untreated chronic conditions. Delayed or forgone treatment for conditions like asthma, diabetes, or even dental problems can lead to significant long-term health complications, increased hospitalizations, and reduced quality of life. For example, untreated childhood asthma can lead to permanent lung damage, impacting respiratory health throughout adulthood.
Similarly, untreated dental problems can lead to infections and systemic health issues. These untreated conditions can also impact school attendance and participation, further compounding the negative consequences.
Impact on Educational Attainment and Future Economic Prospects
The link between health and education is undeniable. Children who experience frequent illnesses or chronic health problems due to lack of healthcare often miss more school, leading to lower academic performance and reduced educational attainment. This, in turn, limits their future employment opportunities and earning potential. Studies have consistently shown a correlation between childhood health and adult socioeconomic status; children who lack access to consistent healthcare are more likely to experience lower incomes and increased poverty in adulthood.
The financial burden of medical debt, often incurred by families struggling to afford healthcare for their children, can also significantly impact family stability and a child’s ability to focus on their education. For instance, a child repeatedly missing school due to untreated illnesses might fall behind academically, limiting their college options and future career prospects.
Societal Costs Associated with Uninsured Children
The societal costs associated with uninsured children are substantial and far-reaching. These costs include increased healthcare expenditures due to delayed treatment and more severe illnesses requiring more extensive and expensive interventions later in life. There are also significant costs associated with lost productivity due to reduced educational attainment and lower employment rates among adults who lacked childhood healthcare access.
The increased burden on the social safety net, including welfare programs and emergency room visits, adds to the overall economic burden. For example, a child with untreated childhood diabetes might require significantly more expensive care later in life, leading to higher healthcare costs for society as a whole. This contrasts with the cost-effectiveness of preventative care, which could have been provided under a consistent healthcare plan.
The looming threat of Medicaid redeterminations and potential CHIP coverage loss for children is deeply concerning. It’s a crisis exacerbated by the already strained healthcare system, highlighted by the recent new york state nurse strike NYSNA Montefiore Mount Sinai , which underscores the critical need for adequate staffing and resources. These issues are interconnected; without sufficient healthcare workers, vulnerable children risk losing access to vital care even further jeopardizing their health.
Visual Representation of the Cascading Effects of Coverage Loss
A visual representation could be a flowchart or a cascading diagram. The top of the diagram would show “Loss of Medicaid/CHIP Coverage”. This would branch into several boxes representing immediate consequences: “Delayed or Forgone Preventative Care,” “Untreated Illnesses/Injuries,” “Increased Absenteeism from School.” Each of these would then branch further, leading to long-term effects: “Poorer Health Outcomes (e.g., chronic conditions),” “Lower Educational Attainment,” “Reduced Employment Opportunities,” “Increased Healthcare Costs for Society,” and “Lower Lifetime Earnings.” The final box could represent the overall impact: “Reduced Quality of Life and Increased Societal Burden.” Arrows connecting the boxes would visually demonstrate the cascading nature of the consequences, illustrating how one problem leads to another, creating a cycle of negative impacts.
The visual would clearly show how a seemingly small initial event (loss of coverage) can have enormous and long-lasting repercussions on an individual child and society as a whole. The use of different colors to represent immediate versus long-term consequences would enhance clarity and impact.
Ultimate Conclusion: Medicaid Redeterminations Children Coverage Loss Chip
Navigating the world of Medicaid and CHIP redeterminations can feel like navigating a maze, especially for families already juggling multiple challenges. The potential loss of healthcare coverage for children is a serious issue with far-reaching consequences. However, by understanding the process, advocating for improvements, and utilizing available resources, we can work towards a system that prioritizes the health and well-being of all children.
Let’s keep the conversation going and push for change.
Helpful Answers
What happens if my child loses Medicaid coverage during redetermination?
Losing coverage can lead to delayed or forgone medical care, impacting their health and development. Explore options like CHIP or marketplace plans immediately.
How can I appeal a Medicaid or CHIP denial?
Each state has a specific appeals process. Contact your state’s Medicaid agency for details and assistance. Don’t hesitate to seek help from advocacy groups.
What if I can’t afford the premiums for a marketplace plan after losing Medicaid?
Subsidies are available to lower costs based on income. Explore the Healthcare.gov website or contact a marketplace navigator for assistance.
My child’s circumstances have changed. Do I need to report this to Medicaid?
Yes, it’s crucial to report any changes in income, address, or family size promptly to maintain eligibility. Failure to do so could lead to coverage loss.