Does Maida Stick to Your Gut Myth or Fact?
Does maida stick to your gut myth or fact – Does maida stick to your gut: myth or fact? This question, swirling around kitchen tables and online forums, deserves a closer look. We’re diving deep into the world of refined wheat flour, exploring its impact on digestion, gut health, and overall well-being. From the science of its composition to individual experiences and healthier alternatives, we’ll uncover the truth behind this common concern and arm you with the knowledge to make informed choices about your diet.
This post will explore maida’s digestive process, comparing it to whole wheat flour and examining its potential to cause digestive distress. We’ll also discuss the gut-brain connection, inflammation, and how different dietary habits influence individual responses to maida. Finally, we’ll look at healthier flour alternatives and their benefits for gut health.
Maida’s Composition and Digestion
Maida, also known as refined wheat flour, is a staple in many cuisines. However, its impact on gut health is a subject of ongoing discussion. Understanding its composition and how it’s digested is crucial to assessing its effects.Maida is primarily composed of starch, with a significant portion of its bran and germ removed during processing. This refinement strips away much of the fiber, vitamins, and minerals naturally present in whole wheat.
The remaining starch consists mainly of amylose and amylopectin, complex carbohydrates that provide energy. It also contains small amounts of protein, but lacks the significant quantities of fiber and micronutrients found in whole wheat.
The Digestive Process of Maida and its Impact on the Gut Microbiome
The digestive process of maida begins in the mouth with enzymatic breakdown of starch. However, the absence of fiber in maida means it’s rapidly digested and absorbed in the small intestine. This rapid absorption leads to a swift spike in blood sugar levels, potentially contributing to insulin resistance in susceptible individuals. Furthermore, the lack of fiber means less prebiotic material for the beneficial bacteria in the gut microbiome.
A healthy microbiome relies on diverse fiber sources to thrive. The limited fiber in maida may therefore contribute to a less diverse and potentially less robust gut microbiome. This can indirectly impact overall gut health and potentially contribute to digestive issues in some individuals.
Comparison of Maida and Whole Wheat Flour Digestibility
Whole wheat flour, unlike maida, retains its bran and germ. This means it’s significantly richer in fiber, which slows down digestion. The fiber acts as a bulking agent, promoting healthy bowel movements and feeding the beneficial bacteria in the gut. This slower digestion leads to a more gradual release of glucose into the bloodstream, preventing the sharp spikes associated with maida consumption.
The presence of fiber in whole wheat also improves satiety, making you feel fuller for longer. In contrast, maida’s rapid digestion often leads to hunger pangs shortly after consumption. This difference in digestibility is a key factor contributing to the differing effects of maida and whole wheat flour on gut health.
Digestive Discomfort and Maida Sensitivity
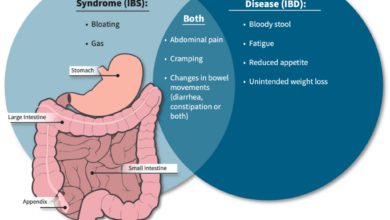
Individuals with pre-existing digestive sensitivities, such as irritable bowel syndrome (IBS) or gluten intolerance (celiac disease), may experience discomfort after consuming maida. While maida itself doesn’t contain gluten in the same way as whole wheat (the gluten proteins are still present, but the structure is altered by processing), its rapid digestion and lack of fiber can exacerbate symptoms in those with sensitive digestive systems.
So, the “maida sticks to your gut” thing – is it true? I’ve been researching gut health lately, and it’s surprisingly complex. It made me think about other health choices, like the decisions women make regarding their reproductive health, for example, learning about Karishma Mehta’s experience with egg freezing and the risks involved, as detailed in this article: karishma mehta gets her eggs frozen know risks associated with egg freezing.
It highlights how important it is to be informed about all our choices, whether it’s about diet or fertility. Back to maida, though – I’m still investigating!
The resulting inflammation and changes in gut microbiota composition may contribute to bloating, gas, and abdominal pain. For individuals with celiac disease, even trace amounts of gluten can trigger an autoimmune response leading to significant digestive issues. While maida is less likely to trigger a severe reaction compared to whole wheat in celiac patients, it can still cause discomfort.
Therefore, individuals with such sensitivities might benefit from avoiding or limiting maida consumption.
The Gut-Brain Connection and Maida Consumption: Does Maida Stick To Your Gut Myth Or Fact
Our gut isn’t just responsible for digestion; it plays a crucial role in our overall health and well-being, influencing everything from mood and sleep to immunity and even cognitive function. This intricate relationship, known as the gut-brain axis, highlights the profound connection between the gut microbiome and the brain. A healthy gut, teeming with diverse beneficial bacteria, contributes significantly to a healthy mind and body.
Conversely, an imbalanced gut microbiome, often characterized by inflammation, can negatively impact various aspects of health.The gut-brain connection operates through various pathways, including the vagus nerve (a direct communication line between the gut and brain), the immune system, and the production of neurotransmitters (chemical messengers) in the gut. Disruptions to this delicate balance can lead to a cascade of problems.
Gut Inflammation and Maida Consumption
Maida, a refined flour stripped of its bran and germ, lacks the fiber and nutrients found in whole grains. This deficiency can contribute to gut inflammation. The lack of fiber disrupts the gut microbiome, potentially leading to an overgrowth of harmful bacteria and an imbalance in the gut flora. Furthermore, the rapid digestion of maida causes blood sugar spikes and crashes, potentially triggering inflammatory responses in the body.
The absence of essential nutrients also weakens the gut lining, making it more susceptible to inflammation and leaky gut syndrome.
So, the “maida sticks to your gut” thing – is it true? I’ve been researching gut health lately, and it’s fascinating how much we still don’t know. It’s a bit of a tangent, but I just read about the FDA approving clinical trials for pig kidney transplants in humans – check it out: fda approves clinical trials for pig kidney transplants in humans – pretty amazing advancements in organ transplantation! Anyway, back to maida – I’m still trying to figure out the science behind that gut-clinging claim.
Gut-Related Symptoms Associated with High Maida Diet
A diet high in maida can manifest in various gut-related symptoms. These can include bloating, gas, constipation, diarrhea, abdominal pain, and even irritable bowel syndrome (IBS) in susceptible individuals. The lack of fiber in maida leads to slower bowel movements and can contribute to constipation. Conversely, the rapid release of sugars can lead to diarrhea in some cases. These symptoms can be further exacerbated by the inflammatory response triggered by maida consumption.
Comparative Effects of Maida and Whole Grain Intake on Gut Inflammation
| Factor | Maida Consumption | Whole Grain Consumption |
|---|---|---|
| Fiber Content | Low | High |
| Gut Microbiome Balance | Potentially Disrupted | Promotes Balanced Microbiome |
| Gut Inflammation | Increased Risk | Reduced Risk |
| Blood Sugar Levels | Spikes and Crashes | More Stable |
Individual Responses to Maida

Source: media-amazon.com
Maida, refined wheat flour, doesn’t affect everyone the same way. Individual tolerance varies significantly, leading to a wide spectrum of digestive and other health experiences. This variability highlights the complex interplay between genetics, gut microbiome, overall diet, and lifestyle factors. Understanding these influences is crucial for navigating a healthy relationship with maida-containing foods.Factors influencing individual tolerance to maida are multifaceted.
Genetic predisposition plays a role, with some individuals possessing a higher capacity to digest gluten, the protein found in wheat, than others. The composition of one’s gut microbiome, the community of bacteria and other microorganisms residing in the digestive tract, is another significant factor. A diverse and healthy gut microbiome aids in digestion and nutrient absorption, potentially mitigating negative effects of maida.
Dietary habits, including the overall frequency of maida consumption and the presence of other foods that might interact with maida’s digestion, also play a critical role. Finally, lifestyle factors like stress levels and overall health status can influence how the body responds to maida.
Varied Responses to Maida Consumption
Individual experiences with maida consumption range widely. Some individuals can consume maida-based products regularly without apparent adverse effects. Others might experience mild discomfort such as bloating or gas, while a smaller percentage might suffer from more severe symptoms like abdominal pain, diarrhea, or even an autoimmune reaction like celiac disease. For example, a person with a history of digestive issues might experience significantly more discomfort after consuming a naan bread compared to someone with a robust digestive system and a diet rich in fiber.
Conversely, someone who regularly consumes fermented foods may exhibit better tolerance to maida due to a more diverse gut microbiome capable of better processing complex carbohydrates.
Digestive Experiences Across Dietary Habits
Individuals with diets high in processed foods and low in fiber often show a greater sensitivity to maida. Their gut microbiome might be less diverse and less equipped to handle the rapid fermentation of maida’s simple carbohydrates. This can lead to increased gas production and discomfort. In contrast, individuals who consume a diet rich in fruits, vegetables, and whole grains often demonstrate better tolerance to maida, likely due to a healthier gut microbiome and improved digestive function.
A person following a predominantly plant-based diet, for example, might experience milder symptoms from maida compared to someone who consumes a diet high in saturated fats and refined sugars. This is because a balanced diet supports a healthier gut environment, better equipped to handle the digestive challenges posed by maida.
Health Conditions Exacerbated by High Maida Intake
High consumption of maida can exacerbate several health conditions. For individuals with celiac disease, even small amounts of gluten can trigger an autoimmune response, leading to damage to the small intestine. Those with non-celiac gluten sensitivity may experience digestive symptoms such as bloating, abdominal pain, and diarrhea. Furthermore, a diet high in refined carbohydrates like maida can contribute to weight gain, type 2 diabetes, and cardiovascular disease due to its low fiber content and high glycemic index.
High maida intake is also associated with increased risk of certain inflammatory conditions. For instance, individuals prone to irritable bowel syndrome (IBS) may find their symptoms worsen with increased maida consumption. It’s important to note that these are correlations, and individual responses will vary.
So, the “maida sticks to your gut” thing – is it true? I’ve been researching gut health lately, and it’s surprisingly complex! It got me thinking about how a child’s overall well-being impacts their health, which led me to this fantastic article on strategies to manage Tourette syndrome in children , a condition where managing stress and diet can play a significant role.
Coming back to maida, I think it’s more about the overall impact of refined carbs on digestion than any literal sticking.
Alternative Flour Options and Their Impact
So, we’ve established that maida, while convenient, isn’t the best friend to our gut health. The good news is, there’s a whole world of alternative flours out there, each offering unique nutritional benefits and impacting digestion differently. Let’s explore some popular options and see how they stack up.
Switching to alternative flours can significantly improve your digestive health by providing more fiber, nutrients, and potentially reducing inflammation. The increased fiber content aids in regular bowel movements, promotes a healthy gut microbiome, and can even help manage blood sugar levels. However, it’s important to remember that individual responses can vary.
Alternative Flour Nutritional Comparison
The table below compares the nutritional profiles and potential gut health impacts of several common flour alternatives. Remember that these values can vary depending on the specific brand and growing conditions.
| Flour Type | Fiber Content (per cup) | Nutrient Highlights | Gut Health Impact |
|---|---|---|---|
| Whole Wheat Flour | High | Rich in B vitamins, iron, and magnesium. | Promotes regularity, feeds beneficial gut bacteria. |
| Multigrain Flour | Moderate to High | Variety of nutrients depending on grains included (e.g., oats, barley, rye). | Diverse nutritional profile supports overall gut health. |
| Oat Flour | Moderate to High | Good source of soluble fiber (beta-glucan), which can lower cholesterol and improve gut health. | Supports gut lining health, may improve satiety. |
| Almond Flour | Moderate | High in healthy fats, vitamin E, and magnesium. | Generally well-tolerated, but can be high in FODMAPs for some individuals. |
| Coconut Flour | High | High in fiber but lower in protein than other options. | Can be very absorbent, requiring adjustments in recipes. May not be suitable for everyone due to its high fiber content. |
Nutritional Benefits of Alternative Flours
Compared to maida, which is essentially refined carbohydrate with minimal nutritional value, alternative flours are packed with vitamins, minerals, and fiber. This nutrient-rich profile contributes to a healthier gut microbiome, better digestion, and improved overall well-being. For example, whole wheat flour’s high fiber content promotes regular bowel movements, preventing constipation, while oat flour’s beta-glucan can help regulate blood sugar levels, benefiting both gut and systemic health.
Improving Gut Health with Flour Substitutions, Does maida stick to your gut myth or fact
Substituting maida with alternative flours can significantly improve gut health. The increased fiber intake feeds beneficial gut bacteria, promoting a balanced microbiome crucial for digestion and immunity. The presence of various vitamins and minerals further supports overall gut function. For instance, switching from maida roti to whole wheat roti can lead to improved regularity and reduced bloating for many individuals.
Similarly, using oat flour in baking can contribute to better blood sugar control and improved satiety.
Preparing Dishes with Alternative Flours
Many recipes can be easily adapted to incorporate alternative flours. For instance, you can substitute up to half the maida in a cake recipe with oat flour for a slightly denser, healthier cake. When using whole wheat flour in bread making, you might need to add a little extra liquid, as it absorbs more moisture than maida. Almond flour works well in gluten-free baking, particularly in cookies and muffins.
Experimentation is key! Start with small substitutions to find the perfect balance for your taste and digestive system.
For example, a simple substitution involves making chapatis using whole wheat flour instead of maida. The preparation method remains largely the same; the only difference is the type of flour used. This simple swap offers significant improvements in nutritional value and gut health.
Visual Representation of Maida’s Impact

Source: imimg.com
Understanding the effects of maida (refined wheat flour) on gut health requires visualizing the changes it can induce at both macroscopic and microscopic levels. While we cannot directly see these changes without advanced medical imaging, descriptive comparisons can help us grasp the potential consequences.A healthy gut lining is characterized by a smooth, even surface, resembling a tightly woven tapestry.
The cells are closely packed, forming a robust barrier against harmful substances. Imagine a lush, green meadow, with healthy, vibrant plants growing close together. This strong barrier ensures efficient nutrient absorption and prevents the leakage of gut contents into the bloodstream. In contrast, a gut lining potentially damaged by high maida consumption might appear more irregular and inflamed.
Think of a patchy, brown lawn with bare patches and weeds poking through. The cellular structure might be compromised, with gaps appearing between cells, allowing for increased intestinal permeability (“leaky gut”). This compromised barrier can lead to inflammation and potential immune responses.
Microscopic Differences in Gut Microbiota
The microscopic world of the gut microbiota also undergoes significant shifts in response to dietary changes. A diverse and balanced gut microbiome, thriving on whole grains, resembles a vibrant rainforest ecosystem. Numerous species of bacteria, fungi, and other microorganisms coexist, each playing a vital role in maintaining gut health. These beneficial microbes produce short-chain fatty acids (SCFAs), which nourish the gut lining and support immune function.
The abundance of different microbial species contributes to a robust and resilient ecosystem. In contrast, a gut microbiome heavily influenced by a diet high in maida might show a less diverse composition. Imagine a barren landscape, dominated by a few hardy species, lacking the richness and complexity of a healthy ecosystem. The dominance of certain bacterial strains, potentially those associated with inflammation, may result in an imbalance, known as dysbiosis.
This reduced diversity can compromise the overall function of the gut microbiome, affecting digestion, nutrient absorption, and immune regulation. The reduced SCFA production further weakens the gut barrier and can contribute to inflammation. The lack of prebiotic fiber in maida, unlike in whole grains, directly contributes to this microbial imbalance.
Concluding Remarks
So, does maida stick to your gut? The answer isn’t a simple yes or no. While maida itself doesn’t literally “stick,” its refined nature can lead to digestive issues for many. Understanding its composition and how it affects your gut microbiome is key. By choosing whole grains and exploring alternative flours, you can promote a healthier gut and improve your overall well-being.
Remember, listening to your body and making dietary choices that support your individual needs is crucial for optimal health.
Expert Answers
What are the long-term effects of a high-maida diet?
Long-term consumption of a high-maida diet can increase the risk of chronic inflammation, weight gain, and digestive problems. It may also contribute to nutrient deficiencies due to the lack of fiber and other essential nutrients found in whole grains.
Can I still eat some maida occasionally?
Occasional consumption of maida is unlikely to cause significant harm for most people. However, prioritizing whole grains as your primary source of carbohydrates is generally recommended for better gut health.
Are there any specific tests to determine maida sensitivity?
There isn’t a single definitive test for maida sensitivity. However, a doctor can conduct tests to rule out other conditions and assess your digestive health. An elimination diet, where you temporarily remove maida from your diet and observe the effects, can also be helpful.
How can I gradually reduce my maida intake?
Start by gradually substituting maida with whole wheat flour or other alternatives in recipes. Begin with a small percentage substitution and gradually increase it over time. Experiment with different recipes and find alternatives you enjoy.